
Essential aspects of left-sided thrombectomy include
starting with the patient in the right-side-up position to
address the caval thrombus first, transient vascular control
of the right renal artery and vein while preserving the right
adrenal gland, followed by thrombectomy, caval recon-
struction, and right renal revascularization. We performed
angioembolization 24 hours preoperatively in 80% of our
patients, especially in those with left-sided or larger tumors.
Preoperative renal embolization has been controversial
prior to open surgical IVC thrombectomy, correlated with
increased transfusions, operative time, and postoperative
complications, leading to longer intensive care unit stay and
higher perioperative mortality
[15]. However, we did not
notice any such downside; rather, it is our impression that
angioinfarction decompressed the venous collaterals, de-
creasing blood loss and enhancing robotic efficacy. Due to
our limited sample size, we are unable to compare
outcomes between those who did and did not undergo
angioembolization.
Our study has limitations. To our knowledge, reported
here is the largest number of robot-assisted level III IVC
thrombectomy cases (
n
= 11) in the literature; nevertheless
it still is a relatively small patient cohort. Also, our median
follow-up of 16
[5_TD$DIFF]
mo is short. We are therefore unable to
report on the long-term oncologic efficacy of robotic
surgery; however, to date the oncologic outcomes have
been sanguine. Given the lack of a comparator open surgical
cohort, we are unable to comment definitively on the
relative merits and demerits of a matched comparison with
open surgery. In this regard, we are currently in the midst of
a retrospective comparison of open and robot-assisted level
II–III IVC thrombectomy.
5.
Conclusions
Our report demonstrates the University of Southern Cali-
fornia technique and clinical outcomes data for robotic level
II–III inferior vena cava tumor thrombectomy. Our encour-
aging early experience provides confidence that the requisite
vascular, reconstructive, and oncologic surgical principles
and technical nuances can be reliably and reproducibly
addressed robotically with good clinical outcomes.
Conflicts of interest
Mihir M. Desai declares conflict of interest for Hansen Medical; Auris
Robotics; Procept Biorobotics; Baxter.
Inderbir S. Gill declares conflict of interest for EDAP, Mimic, Hansen
Medical.
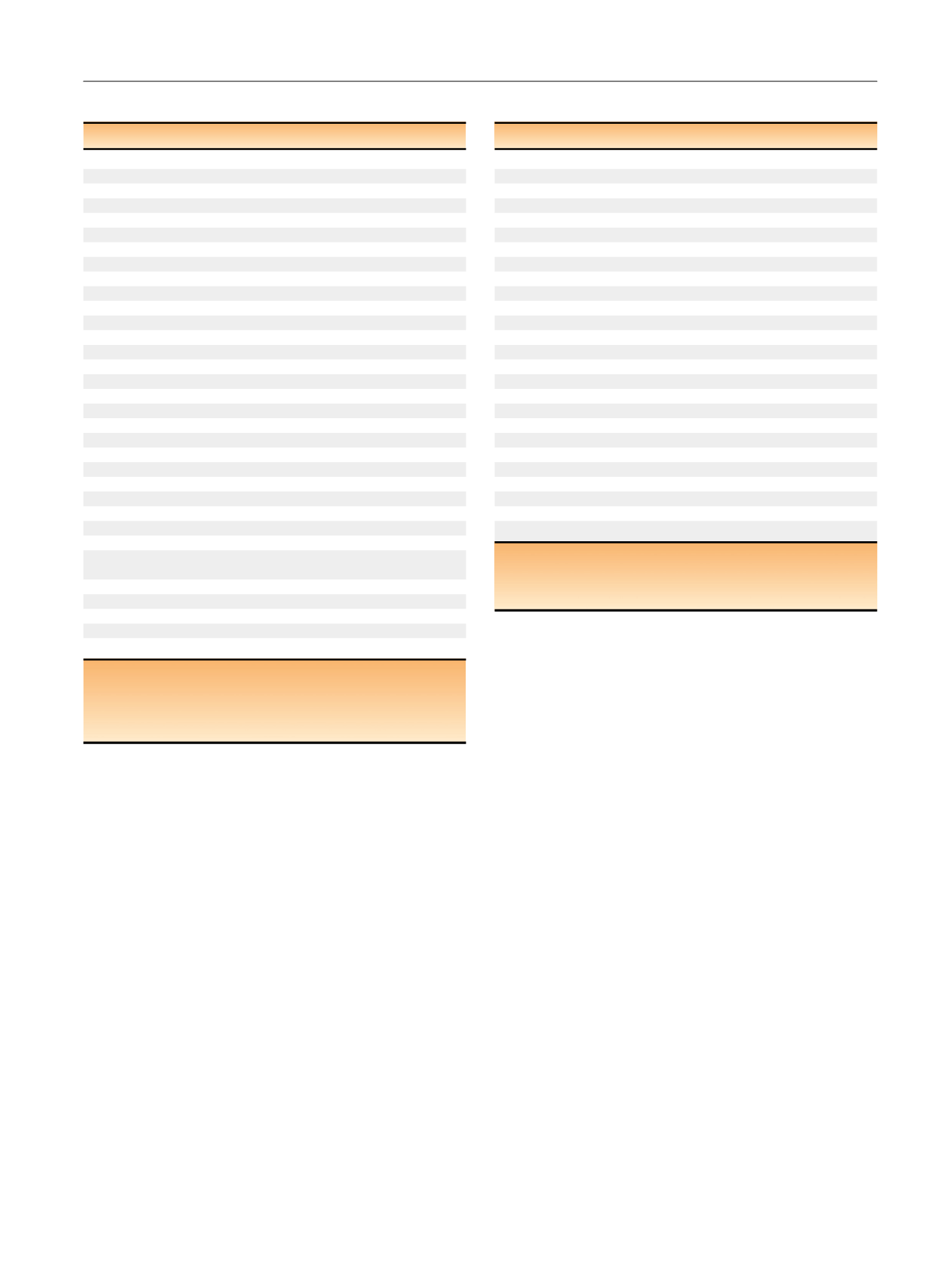
Table 1 – Demographic and perioperative data
Variable
Results
Patients,
n
24
Age, yr, median (range)
64 (36–88)
Male,
n
(%)
21 (87.5)
BMI, kg/m
2
, median (range)
28 (22–41.9)
ASA score, median (range)
3 (2–4)
Charlson Comorbidity Index, median (range)
2 (0–6)
Renal tumor
CT size, cm, median (range)
8.5 (5.3–19.5)
Left side,
n
(%)
7 (29.2)
IVC thrombus length, cm, median (range)
4 (2–7)
Mayo IVC thrombus classification level,
n
(%)
II
13 (54.2)
III
11 (45.8)
Preexisting metastasis,
n
(%)
5 (20.8)
Neoadjuvant therapy,
n
(%)
2 (8.3)
*Preoperative embolization,
n
(%)
20 (80.3)
Operative time, h, median (range)
4.5 (3–8)
Thrombectomy time, h
2.6 (1.3–5)
IVC clamp time, h
0.4 (0.3–1.7)
Nephrectomy time, h
1 (0.3–3)
RPLND time, h
0.5 (0.3–1.5)
Hepatic veins taken, median (range)
1.5 (0–5)
Proximal caval control
Suprarenal IVC
Intrahepatic,
n
(%)
9 (37.5)
EBL, ml, median (range)
240 (100–7000)
Patients receiving intraoperative transfusions,
n
(%)
5 (20.8)
Patients receiving intraoperative bovine pericardial
patch,
n
(%)
1 (4.2)
Lymph nodes removed, median (range)
7 (1–22)
Lymph nodes positive, median (range)
0 (0–22)
Intraoperative complications,
n
0
Positive surgical margins,
n
0
Length of hospital stay, d, median (range)
4 (1–22)
ASA = American Society of Anesthesiologists; BMI = body mass index;
CT = computed tomography; EBL = estimated blood loss; IVC = inferior
vena cava; RPLND = retroperitoneal lymph node dissection.
*
One patient underwent tyrosine kinase inhibitor treatment for 3 mo; one
patient underwent partial nephrectomy.
Table 2 – Pathology and follow-up data
Variable
Results
Patients,
n
24
Histology,
n
(%)
Renal cell carcinoma
23 (95.8)
Papillary type II
1 (4.2)
Tumor grade,
n
(%)
2
7 (29.2)
3
11 (45.8)
4
6 (25.0)
Stage,
n
(%)
T3a
5 (20.9)
T3b
14 (58.3)
T3c
2 (8.3)
T4a
3 (12.5)
Positive lymph nodes,
n
(%)
3 (12.5)
No. of patients with 1-yr Clavien complications,
n
(%)
4 (16.7)
2
2 (8.3)
*3a
1 (4.2)
y
3b
1 (4.2)
z
Cancer status
Disease free
13 (54.2)
Recurrence
11 (45.8)
Patient status,
n
(%)
Alive
24 (100)
Dead
0
Adjuvant therapy,
n
(%)
10 (41.7)
Follow-up, mo, median (range)
16 (12–39)
*
Pulmonary embolism or deep vein thrombosis (treated with nadroparin;
occurred within 90 d after surgery).
y
Chylous ascites.
z
Percutaneous drainage of subphrenic abscess.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 6 7 – 2 7 4
273
















