
and T4a (
n
= 3). Three patients (12.5%) were found to have
positive lymph nodes. Median follow-up for the cohort was
16 months (range: 12–39months). All patients were alive at
last follow-up. Eleven patients (46%) developed new-onset
metastatic disease; at last follow-up, 10 patients (42%) had
received adjuvant therapy.
4.
Discussion
Level III IVC tumor thrombectomy is one of the most
challenging open surgical urologic oncologic procedures,
with major complication rates of up to 38% and periopera-
tive mortality rates of 4–10%
[8]. Given the potential for
these major intraoperative complications, it is essential
that the perioperative safety, oncologic efficacy, and
technical reproducibility of the robotic approach be
carefully documented before integration and eventual
adoption at other centers of robotic expertise. At our
institution, a backup open surgical team is on standby in
the event of an intraoperative complication. We also pre-
prepare so-called rescue stitches
[14] ,made of a 6-inch-
long suture of 2-0 Vicryl (Ethicon, Somerville, NJ, USA) on a
CT-1 needle with a Hem-o-lok tied to the end of the stitch,
which can be used expeditiously to control a bleeding
vessel. Finally, a competent bedside assistant, facile in
laparoscopic suction irrigation, also adds further expertise
in securing vascular control. Most important, careful and
meticulous vascular dissection with precise control of all
feeding blood vessels is paramount for successful out-
comes.
To guard against tumor embolism, a minimal IVC touch
strategy is adopted. To the extent possible, tissues are
dissected away from the IVC, rather than the IVC away from
the tissues. Immediately after securing the thrombus-
bearing IVC segment by tightening the Rummel tourniquets
(thus eliminating any chance of embolization), we staple-
transect the thrombus-bearing renal vein. This key step
delivers three major advantages: (1) The thrombus-bearing
caval segment can now be easily rotated and inspected 360
8
to ensure all feeding lumbar veins are clipped; (2) back
bleeding from the tumorous kidney into the IVC is
eliminated; and (3) the excised thrombus and stapled renal
vein ostium are immediately placed in the Endo Catch bag,
precluding local spillage.
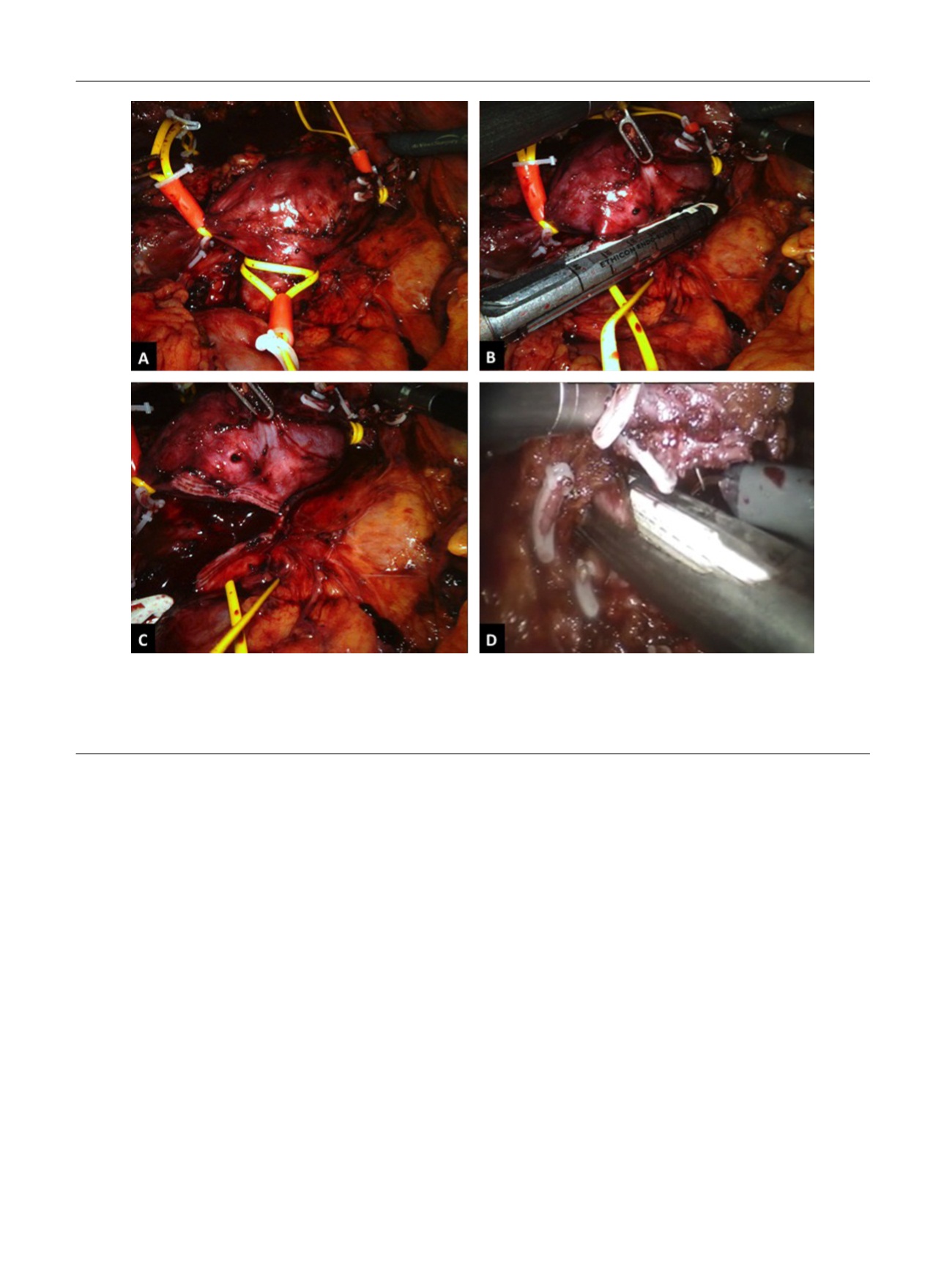
[(Fig._4)TD$FIG]
Fig. 4 – Left-sided caval thrombectomy. (a) The infrarenal inferior vena cava (IVC), suprarenal IVC, left and right renal veins are encircled with a
double-loop tourniquet and secured with a Hem-o-lok clip. Then the right renal artery and right renal vein are controlled using individual bull-dog
clamps. (Note: In this operative picture, the patient had a solitary kidney. The previous kidney was emergently removed during a previous motor
vehicle accident). (b, c) The thrombus-bearing left renal veins is transected with an Endo GIA stapler after have already undergone preoperative
angioembolization. (d) The left renal artery is ligated following patient repositioning.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 6 7 – 2 7 4
272
















