
relevant number of short hepatic veins is controlled with
robotic Hem-o-lok clips and/or suture-ligation
( Fig. 2 g).
Releasing the short hepatic veins is essential to retract the
caudate lobe; this maneuver exposes an additional 3–4 cm
of the IVC allowing high intrahepatic access to the retro-
hepatic IVC. The right main adrenal vein is controlled with
Hem-o-lok clips
( Fig. 2 h), and the right lateral border of the
suprarenal IVC is dissected. Retrocaval dissection of the
intrahepatic IVC is performed. A double-fenestrated grasper
is used to encircle the IVC with a Rummel tourniquet in this
high retrohepatic location
( Fig. 2 i). The right renal hilum is
dissected and the right renal vein is exposed.
2.3.4.
Right-sided caval thrombectomy
All Rummel tourniquets are reconfirmed to be in the
appropriate position, with a sufficient margin around the
thrombus. This is achieved with visual confirmation
(appropriate narrowing of the cava on cinching the Rummel
tourniquet) and/or a drop-in ultrasound probe.
The right renal artery is dissected and clipped in the
interaortocaval region
( Fig. 3a). Anesthesia is alerted that
caval blood flow will be temporarily halted. The initial
maneuver is to cinch the distal (infrarenal) IVC tourniquet.
Once assured that the patient is able to tolerate caval cross-
clamping, the left renal vein and proximal IVC Rummel
tourniquets are cinched sequentially, thus excluding the
thrombus-bearing caval segment. The thrombus-bearing
right renal vein is transected with an Endo GIA stapler
(vascular load; Covidien)
( Fig. 3 band 3c). The excluded
caval segment is now rotated and circumferentially
inspected 360
8
to reconfirm visually that all feeding lumbar
veins have been secured. An appropriately situated
cavotomy is created toward the right edge of the IVC,
adjacent to the right renal vein ostium
( Fig. 3 dand 3e); the
cavotomy should be well planned so that subsequent caval
reconstruction does not overly narrow its lumen.
The thrombus is carefully dissected free from the IVC
lumen without local spillage
( Fig. 3 fand 3g). The right renal
vein ostium, along with its staple line, and any infiltrated or
densely adherent IVC wall are excised en bloc with the
thombus; the tumor thrombus specimen is immediately
placed in a 10-mm Endo Catch bag (Covidien), precluding
local seeding. The IVC lumen is copiously irrigated and
flushed with heparinized water. Caval reconstruction is
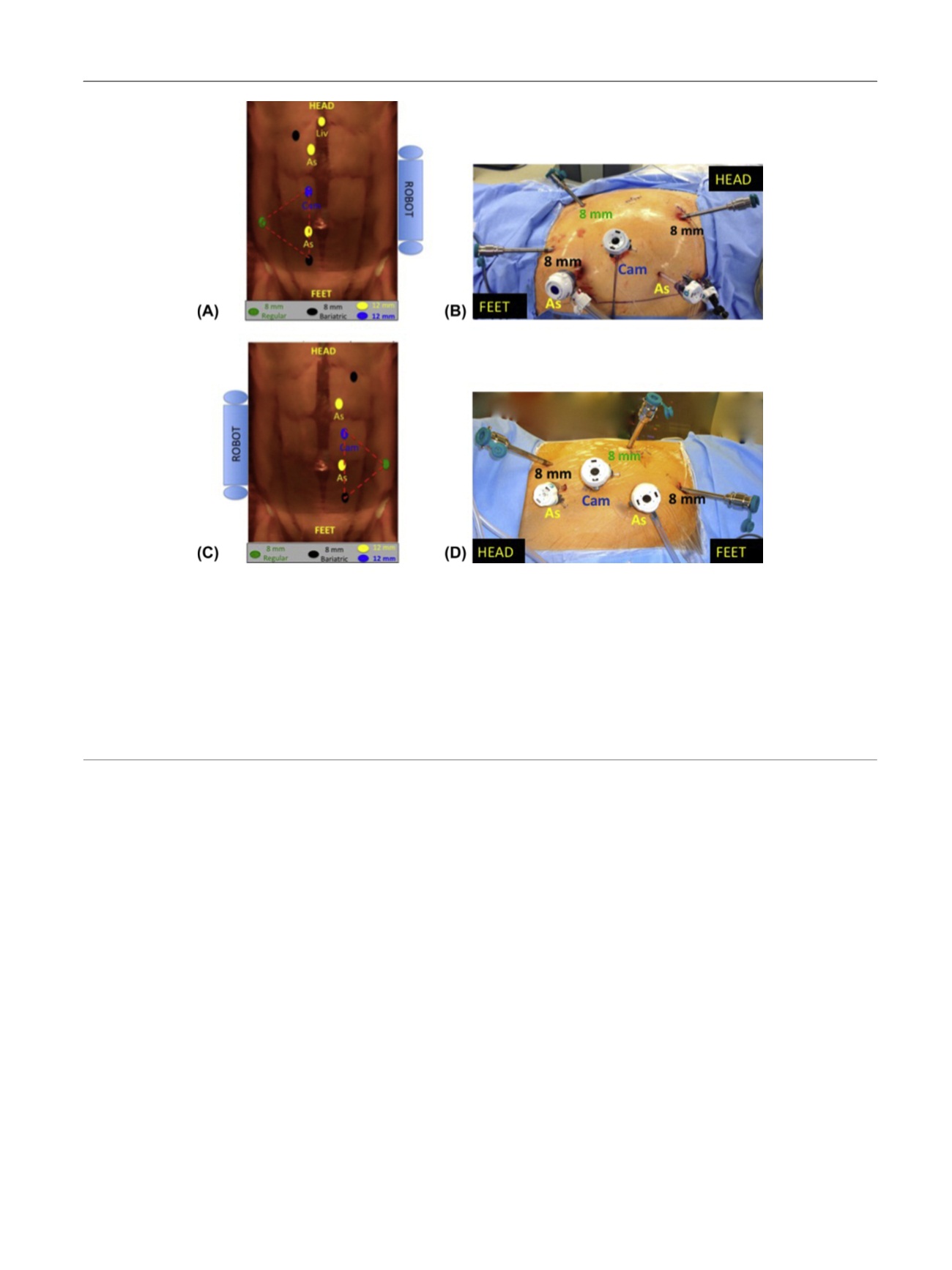
[(Fig._1)TD$FIG]
Fig. 1 – Patient positioning and port placement. Veress needle pneumoperitoneum is achieved, and the 12-mm camera port is placed at the level of the
12th rib in a somewhat more medial location than regular renal robotic surgery, where this port is closer to the right lateral rectus border. The rest of
the bariatric robotic ports are inserted, the most caudal located cephalad to the pubic symphysis and slightly lateral to the medial umbilical ligament.
One robotic port is placed three fingerbreadths cephalad and medial to the anterosuperior iliac spine; of note, an equilateral triangle configuration is
the goal of these three ports (including the camera port). The uppermost bariatric robotic port is placed one fingerbreadth from the costal margin, 8–
10 cm cephalad to the camera port. A 5-mm port is placed below the xiphisternum for liver retraction; a 12-mm assistant port is placed medially
between the camera and uppermost robotic port; and a 15-mm assistant port is placed distal to the umbilicus, closer to the midline. The robot is
docked over the patient’s shoulder. (a) Schematic demonstrating port placement for vena caval control (laterality nonspecific) and right-sided caval
thrombectomy; (b) operative photograph demonstrating port placement for vena caval control (laterality nonspecific) and right-sided caval
thrombectomy; (c) schematic demonstrating port placement for left radical nephrectomy following caval thrombectomy; (d) operative photograph
demonstrating port placement for left radical nephrectomy following vena caval thrombectomy.
As = assistant port; Cam = camera; Liv = liver.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 6 7 – 2 7 4
269
















