
Society of Anesthesiologists score. Preoperative tumor
characteristics included renal tumor size and side, throm-
bus length, and thrombus level (Mayo classification
[13]).
Preoperative embolization status, any preexisting metasta-
sis, and neoadjuvant treatment status are noted. Operative
and postoperative data were collected as per our database
protocol. Median, range, and statistical significance were
used to report continuous and categorical data.
3.
Results
Table 1presents the demographic and perioperative data.
Of the cases, 24 (96%) were successfully completed
robotically without intraoperative complications. One
patient (4%) was electively converted to open surgery
within 30–45 minutes of starting because of failure to
progress due to insurmountable bowel loops. Because the
entire IVC surgery in this case was performed open
surgically for
>
8 h, this case was censured from postopera-
tive analysis.
Of the cases, 11 (46%) were Mayo level III thrombi and
13 were Mayo level II (54%). Primary renal tumors were
right sided (
n
= 16) or left sided (
n
= 7), with median size
8.5 cm (range: 5.3–19.5 cm) on radiologic imaging. Median
thrombus length was 4 cm (range: 2–7 cm). Five patients
(21%) had low-volume preexisting metastasis at the time of
surgery: pulmonary (
n
= 1), paracaval 2.2-cm node (
n
= 1),
lumbar vertebra (
n
= 1), and adrenal gland with two lymph
nodes (
n
= 1). Two patients (8.3%) received neoadjuvant
therapy, with one a prior partial nephrectomy. Twenty
patients (80%) underwent preoperative renal artery embo-
lization. The median number of hepatic veins taken was 1.5
(range: 0–5), median operating time was 4.5 hours (range:
3–8 hours), and estimated blood loss was 240 ml (range:
100–7000 ml).
Table 1summarizes the operative time
breakdown of the procedure steps. Five patients (21%)
required blood transfusion(s). Median hospital stay was
4 days (range: 1–22 days).
Four patients (16.7%) had a complication within 1 year
postoperatively. These included deep vein thrombosis
(
n
= 1) or pulmonary embolus (
n
= 1), both treated with
anticoagulation (Clavien 2), chylous ascites (
n
= 1) treated
with paracentesis (Clavien 3a), and subphrenic abscess
(
n
= 1) treated with percutaneous drainage (Clavien 3b).
Table 2presents the pathology and follow-up data. Final
pathologic stage was T3a (
n
= 5), T3b (
n
= 14), T3c (
n
= 2),
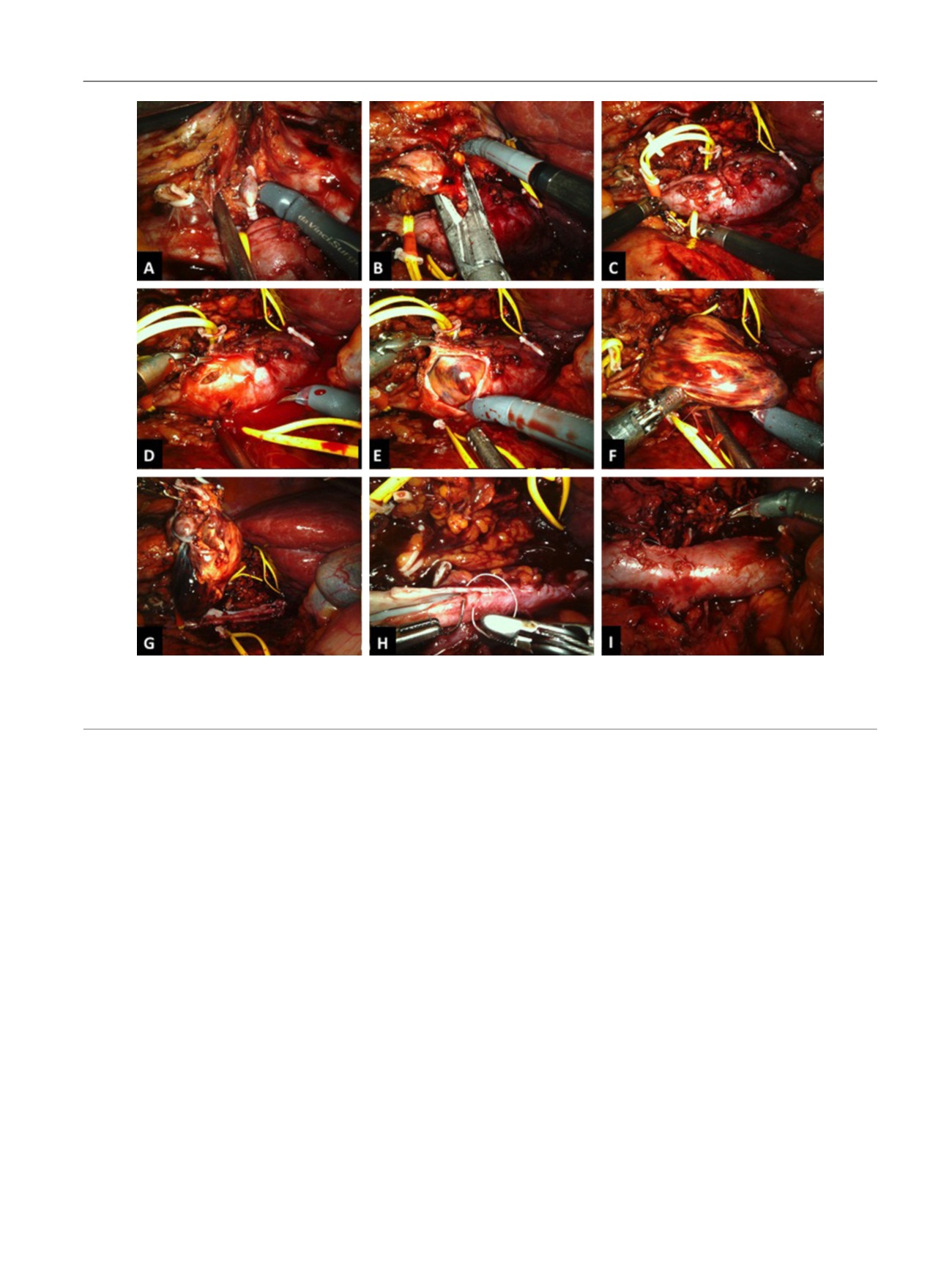
[(Fig._3)TD$FIG]
Fig. 3 – Right-sided caval thrombectomy. (a) The right renal artery is clipped and transected; (b, c) the thrombus-bearing right renal vein is transected
with an Endo GIA stapler; (d–f) a cavotomy is performed and the thrombus is removed; (g) the thrombus is dissected free without local spillage; (h) a
5-0 Gore-Tex suture is used for inferior vena cava reconstruction; (i) the tourniquets are released and caval flow is restored.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 6 7 – 2 7 4
271
















