
1.
Introduction
Efforts to improve the initial accuracy of prostate cancer
(PCa) focus on providing greater certainty with which
clinicians and patients decide on management options such
as active surveillance (AS). In particular, multiparametric
magnetic resonance imaging (mpMRI) has received exten-
sive study as a staging and diagnostic tool
[1] .Platforms
offering real-time MRI-ultrasound fusion have been shown
to substantially minimize initial misclassification while
detecting clinically significant PCa in biopsy-naı¨ve or
undiagnosed men, yet the utility of MRI-ultrasound fusion
technology among patients with known PCa managed with
AS remains unclear
[2–4].
Periodic biopsies evaluating for disease progression are a
central feature of PCa surveillance
[5,6] .Upgrading at
follow-up biopsy and discordances between core needle
biopsy and radical prostatectomy pathology findings
underscore the limitations of initial systematic biopsy
[7,8]. A growing body of evidence supports incorporating
MRI-ultrasound fusion biopsy at diagnosis, including a
prospective study of 1013 patients
[1,3]. Once a diagnosis
has been made, little clinical evidence exists to guide the
use of MRI-ultrasound fusion biopsy. From this perspective,
we aimed to define the rates of Gleason score (GS)
upgrading with MRI-ultrasound fusion biopsy among a
prospectively followed cohort of men with low- and
intermediate-risk PCa managed with AS.
2.
Methods
2.1.
Study design
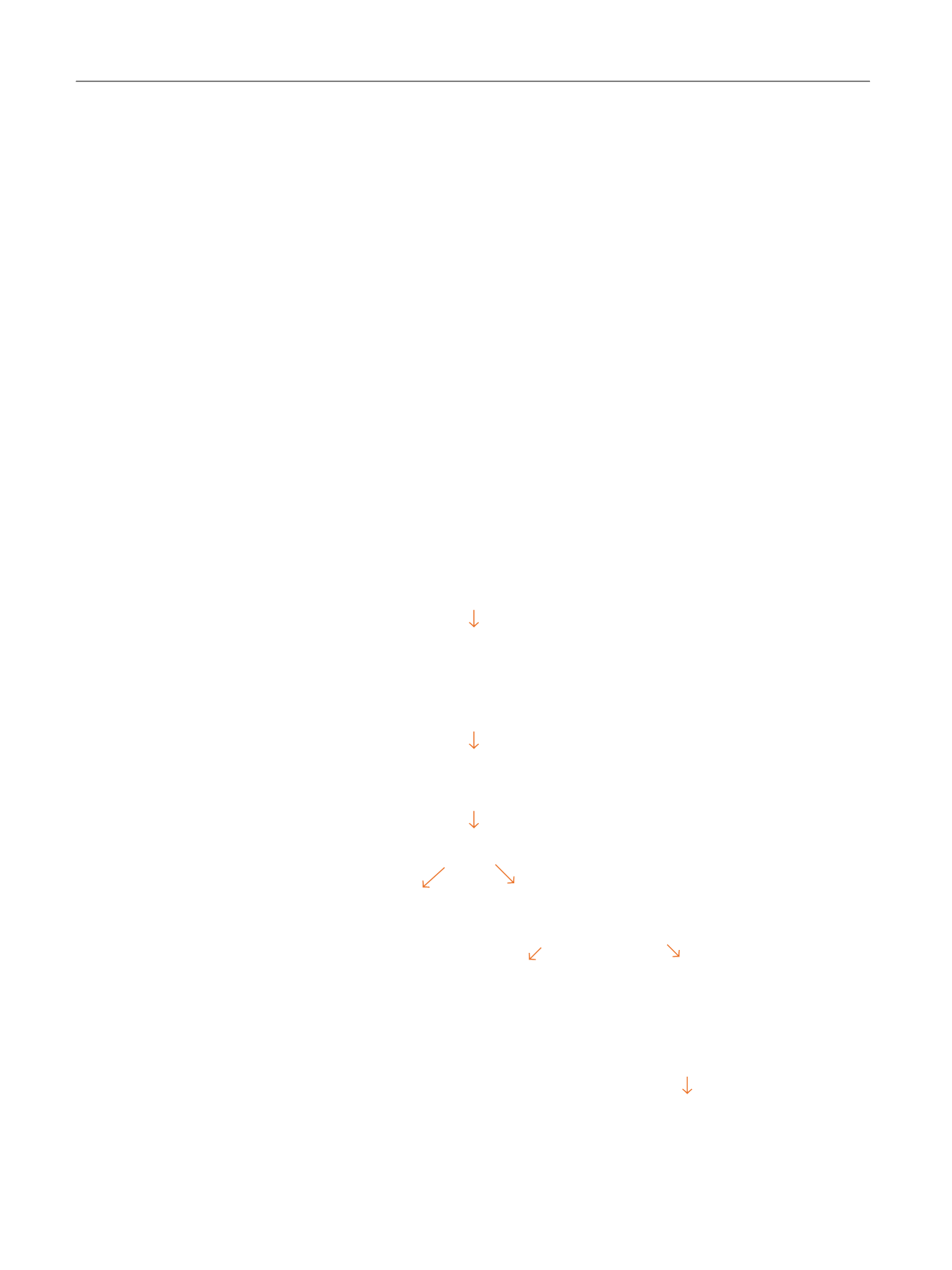
Patients at the University of California, San Francisco (UCSF) diagnosed
with PCa were prospectively enrolled in the Urologic Outcomes Database
(UODB) under institutional review board supervision
( Fig. 1). Through
the UODB, we identified men who received confirmatory or surveillance
MRI-ultrasound fusion biopsy with concurrent systematic biopsy during
AS between July 2014 and December 2015.
All participants had at least one previous transrectal ultrasound
(TRUS)–guided systematic biopsy yielding evidence of PCa, and mpMRI
showing at least one region suspicious for cancer. Strict UCSF inclusion
criteria for AS applied to 76% of our cohort, including a prostate-specific
antigen (PSA) 10 ng/ml, clinical stage T1 or T2, GS sum score 6, 33%
cores positive for malignancy, and no single core containing
>
50% of
tumor
[6,9] .Men with otherwise favorable low- or intermediate-risk
disease outside of strict criteria (24% of our cohort) were selectively
offered AS after extensive risks and benefits counseling
[10]. In addition,
seven patients were excluded because mpMRI was done
>
18 mo before
[(Fig._1)TD$FIG]
UCSF Urologic Outcomes Database December 15, 2015
n
= 5535
Consented for research
n
= 5515
Active surveillance n = 1460
Radical prostatectomy n = 4055
All men who have undergone MRI-ultrasound fusion prostate biopsy since implementation at UCSF (July
2014)
n
= 336
Biopsy indication
noitacidniecnallievruS
noitacidniecnallievrusnoN
n
= 91
n
= 236
Elevated PSA n = 77
Posttreatment imaging n = 14
Excluded
Included
n
= 29
n
= 207
Fusion biopsy findings n =
229
>18 mo from MRI to
biopsy n = 7
Consented for research n =
207
No consent n = 22
Final analytic group
n
= 207
Fig. 1 – Study design evaluating magnetic resonance imaging–ultrasound fusion biopsy among patients with prostate cancer managed with active
surveillance.
MRI = magnetic resonance imaging; PSA = prostate-specific antigen; UCSF = University of California, San Francisco.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 7 5 – 2 8 1
276
















