
fusion cores at the same biopsy session. The model testing likelihood of
any upgrading was restricted to men with systematic biopsy findings
with GS 3 + 3. The major upgrading model included men with
systematic biopsy findings with GS 3 + 4. Independent variables were
selected a priori and assessed for interitem correlations with Pearson’s
R
and linear regression. Variance inflation factors were very low (range:
1.04–1.22) for each independent variable, thus no variable was excluded
from logistic regression modeling due to collinearity. The final set of
covariates at MRI-ultrasound fusion biopsy included age (in years), PSA
level (in nanograms per milliliter), prostate volume (in milliliters),
presence of a hypoechoic lesion on TRUS (yes or no), number of previous
biopsy sessions (continuous), time from mpMRI to MRI-ultrasound
fusion biopsy (in months), number of systematic biopsy cores sampled,
and number of MRI-ultrasound fusion biopsy cores sampled. For each
model, we reported the area under the receiver operating characteristic
curve (AUC) as a measure of model accuracy. A
p
<
0.05 was considered
statistically significant. Analysis was done using SAS v.9.4 (SAS Institute,
Cary, NC, USA) and Stata/IC v.14.1 for Windows (StataCorp, College
Station, TX, USA).
3.
Results
Between July 2014 and December 2015, 326 men with PCa
underwent MRI-ultrasound fusion prostate biopsy at UCSF.
Of them, 236 had biopsy-proven PCa managed with AS;
after exclusions, 207 patients remained in this study
( Fig. 1).
The clinical and demographic characteristics at diagnosis
are summarized in
Table 1. The median PSA level at biopsy
was 5.9 ng/ml (IQR: 4.3–8.8 ng/ml) and the median PSA
density was 0.15 ng/ml per ml (IQR: 0.09–0.21 ng/ml per
ml). The median prostate volume prior to biopsy was 42 ml
(IQR: 31–57 ml). The median number of previous biopsy
sessions was 2 (IQR: 1–3). The median time from mpMRI to
MRI-ultrasound fusion biopsy was 2 mo (IQR: 1–4 mo), and
the median time from previous biopsy to MRI-ultrasound
fusion biopsy was 16 mo (IQR: 10–25 mo). Prior to MRI-
ultrasound fusion biopsy, participants’ most recent GSs
were negative (8%), 3 + 3 (67%), and 3 + 4 (25%). MRI
suspicion scores were 3/5 for 21%, 4/5 for 56%, and 5/5 for
23%.
All patients received MRI-ultrasound fusion biopsies
with a median of 2 needle cores taken (IQR: 2–4; range:
2–14) and systematic sampling with a median of 14 cores
taken (IQR: 14–14; range: 2–22). The median percentage of
needle cores positive for PCa was 50% (IQR: 0–100%) for
MRI-ultrasound fusion sampling and 21% (IQR: 7–43%) for
systematic sampling. The median maximum tumor in-
volvement was 40% (IQR: 20–64%) in a needle core for MRI-
ultrasound fusion and 31% (IQR: 14–50%) for systematic
biopsy
( Table 2).
MRI-ultrasound fusion biopsy cores alone detected PCa
in 130 patients (63%). 77 patients (37%) had negative MRI-
ultrasound fusion cores, 58 (28%) had GS 3 + 3, 54 (26%)
GS 3 + 4, and 18 (9%) GS 4 + 3 tumors. Systematic cores
were positive in 176 men (86%), including 100 (48%)
with GS 3 + 3, 51 (25%) with GS 3 + 4, and 25 (12%) with
GS 4 + 3 cancers, and they were negative for 31 men (15%).
Across all patients, agreement between systematic GS
and MRI-ultrasound fusion GS approached a threshold for
statistical significance (
p
<
0.047)
( Table 3). Overall, 83 men
(40%) experienced any upgrading, including 49 (24%) from
prior biopsy to current systematic biopsy alone, 30 (14%)
from current systematic biopsy to MRI-ultrasound fusion
cores taken at the same time, and 4 (2%) from prior biopsy to
both current systematic and MRI-ultrasound fusion biopsy
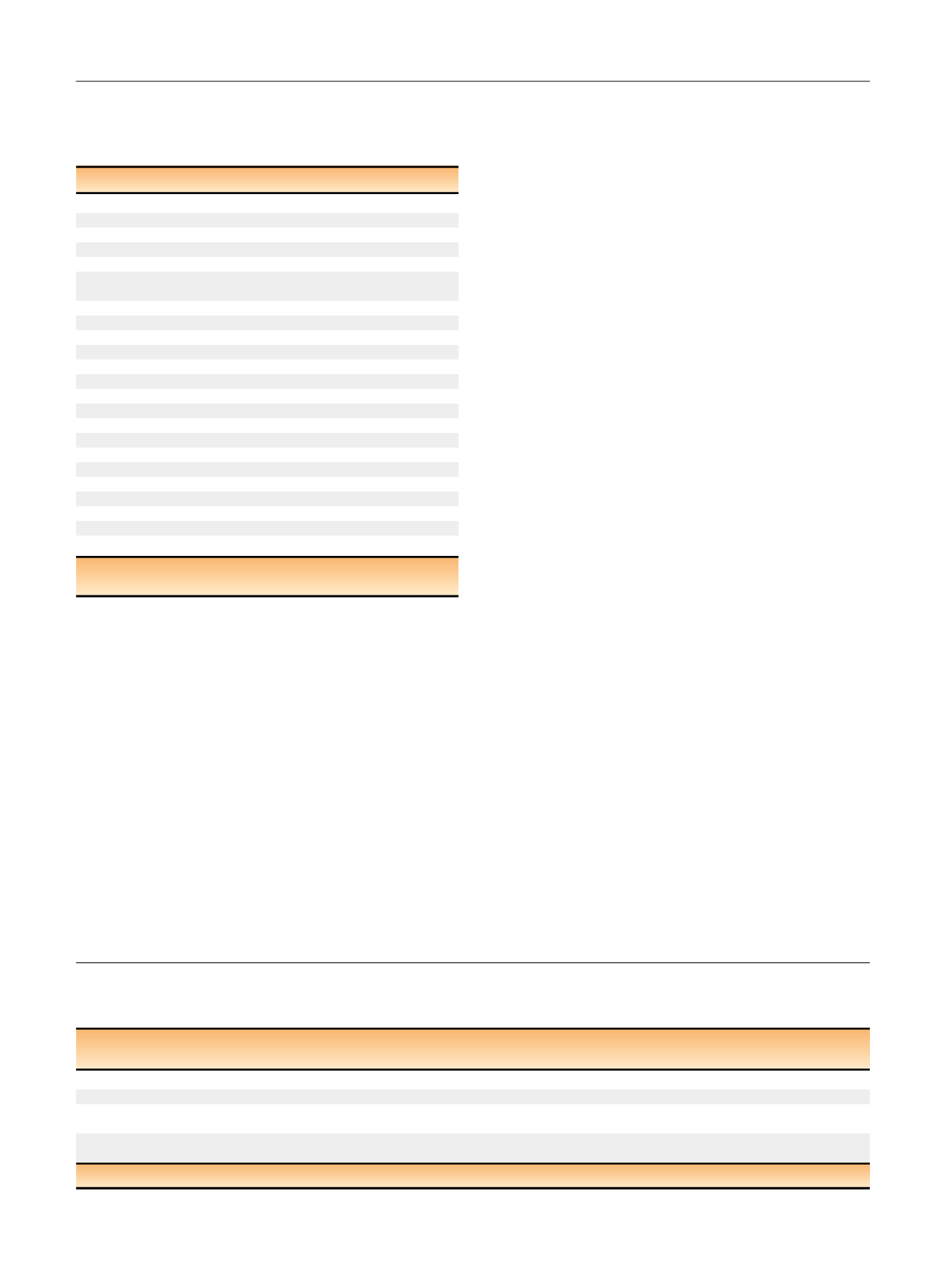
Table 1 – Baseline characteristics of 207 men with active
surveillance for prostate cancer management at the University of
California, San Francisco, who underwent concomitant magnetic
resonance imaging–ultrasound fusion and systematic biopsies
Characteristic
Value
Age, yr, median (IQR)
66.7 (61.4–70.4)
PSA, ng/ml, median (IQR)
5.9 (4.3–8.8)
PSA density, ng/ml/ml, median (IQR)
0.15 (0.09–0.21)
Prostate volume, ml, median (IQR)
42 (31–57)
No. of prior biopsies, median (IQR)
2 (1–3)
Time between last biopsy and MRI-ultrasound
fusion biopsy, mo, median (IQR)
15.72 (9.74–24.77)
Time from MRI to biopsy, mo, median (IQR)
2.21 (0.99–4.03)
Clinical T stage,
n
(%)
T1c
74 (36)
T2a
121 (59)
T2c
11 (5)
MRI suspicion score,
n
(%)
1 (Very low)
4 (2)
2 (Low)
0 (0)
3 (Intermediate)
38 (19)
4 (High)
115 (57)
5 (Very high)
49 (23)
Prior biopsy Gleason score,
n
(%)
Negative
16 (8)
3 + 3
138 (67)
3 + 4
41 (20)
4 + 3
8 (4)
4 + 4
4 (2)
IQR = interquartile range; MRI = magnetic resonance imaging;
PSA = prostate-specific antigen.
Table 2 – Comparison of magnetic resonance imaging–ultrasound fusion and systematic biopsy findings and technique for 207 men with
active surveillance for prostate cancer management at the University of California, San Francisco, who underwent concomitant magnetic
resonance imaging–ultrasound fusion and systematic biopsies
Characteristic
Systematic
biopsy
MRI-ultrasound
fusion biopsy
No. of cores taken, median (IQR) (range)
14 (14–14) (2–22)
2 (2–4) (2–14)
No. of positive cores, median (IQR)
3 (1–6)
2 (0–2)
Percentage of positive cores
among total cores, %, median (IQR)
21 (7–43)
100 (50–100)
Maximum percentage of tumor
involvement in a single core, %, median (IQR)
31 (14–50)
40 (20–64)
IQR = interquartile range; MRI = magnetic resonance imaging.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 7 5 – 2 8 1
278
















