
received an extended lymph node dissection. Ten patients
(91%) had nodal invasion and eight patients (73%; 95% CI,
41–95%) had positive margins at final pathology. Adjuvant
ADT and radiotherapy were administered to 10 (91%) and 7
(64%) patients, respectively. Median follow-up for patients
who did not experience CSMwas 63 mo (95% CI, 48–77 mo).
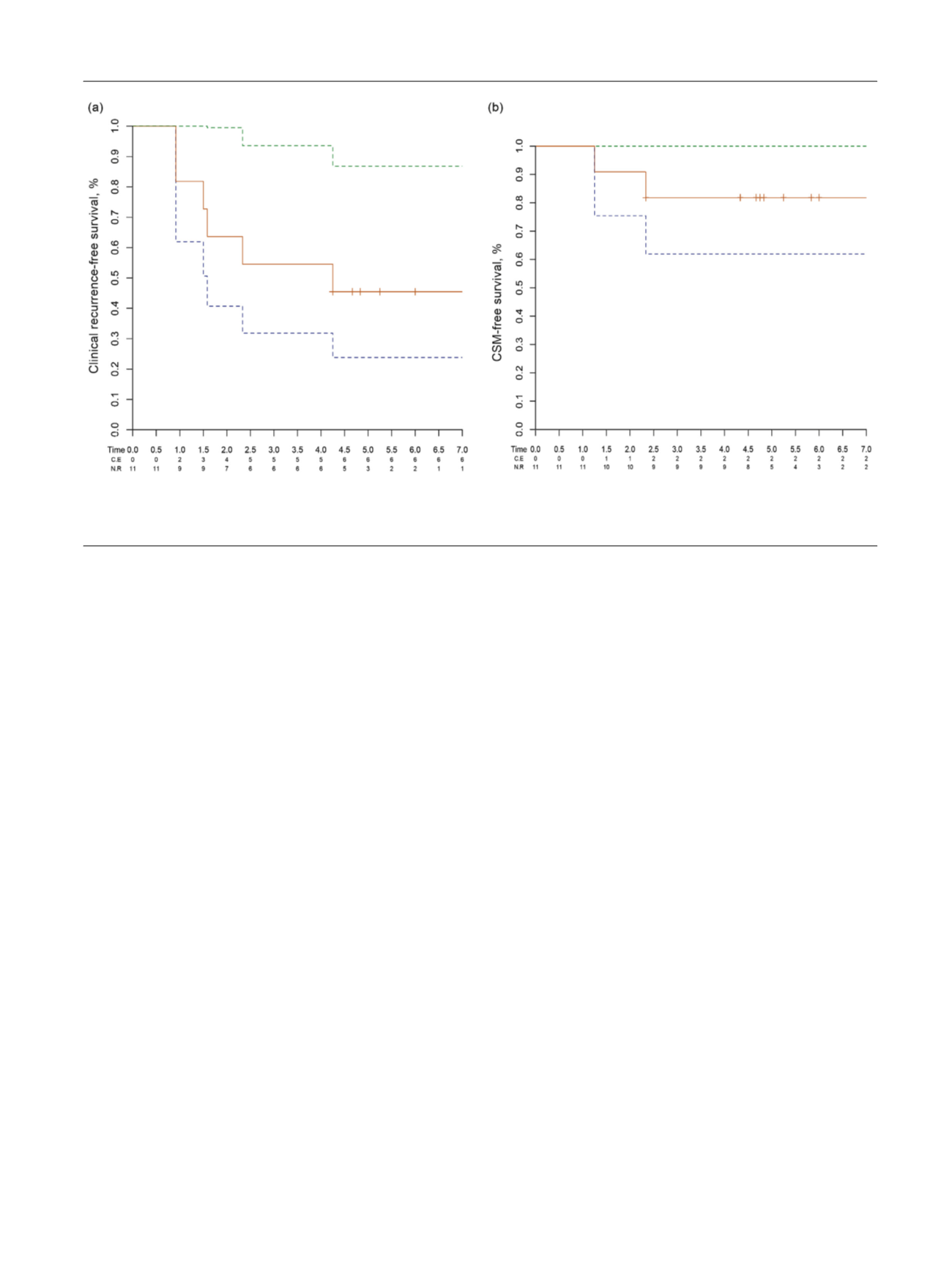
At 7-yr follow-up, 11.1% patients received salvage radio-
therapy. The 7-yr clinical progression- and CSM-free
survival rates were 45% (95% CI, 30–85%) and 82% (95%
CI, 62–99%), respectively
( Fig. 1 ).
The prognosis for men with disseminated metastatic
disease substantially differs compared with those with PCa
limited to the skeleton or the lymph nodes, and a chance of
cure in the latter group might exist
[9–12]. Although the
exact definition of oligometastatic PCa is still debated, these
two categories (polymetastatic vs oligometastatic patients)
could represent biologically different entities. In particular,
patients with oligometastatic disease might harbor an
intermediate state of progression between localized tumor
and widespread metastases
[14]. Removal of the primary
tumor in this setting could delay progression and eventually
affect oncologic outcomes. The rationale for local treatment
in metastatic PCa is supported by preclinical studies
showing that removal of the primary tumor could eliminate
the source of cytokines that facilitate the spread of
metastatic cells. Local treatment could also reduce tumor
burden, improving response to systemic therapies. The
elimination of the principal source of metastatic cells could
limit the proliferation of more aggressive subpopulations of
cancer cells
[1,15]. This evidence together with observation
in metastatic patients affected by other diseases led to the
hypothesis that RP might provide an oncologic benefit in
oligometastatic PCa
[1,3–6]. Population-based studies
demonstrated that metastatic patients who received RP
had improved oncologic outcomes compared with those
who did not receive local treatment
[3,6]. Moreover, a
recent multi-institutional study evaluating men with
metastatic PCa reported acceptable perioperative and
oncologic outcomes, in which almost 90% of patients did
not die from the disease itself at 2-yr follow-up
[5] .Never-
theless, these studies are limited by short follow-up and by
their observational nature, and details on the number and
sites of metastases and on additional cancer therapies were
not always present
[1].
Our investigation focused on a highly selected cohort with
available data on the number and sites of metastases and on
the use of additional cancer therapies. Surgery was
performed in well-selected patients without relevant
comorbidities, according to the clinical judgment of the
treating physician, even in the absence of data supporting the
safety and efficacy of RP in the oligometastatic setting at the
beginning of the study. Nonetheless, observations coming
from preclinical studies
[7]together with evidence support-
ing a rationale for the removal of the primary tumor in
patients with nodal metastases
[16]led to the hypothesis
that RP might play a role in highly selected patients with
oligometastatic PCa. Surgery was associated with an
acceptable safety profile: Only two patients experienced
grade 3 complications, and no perioperative mortality was
recorded. However, intraoperative blood loss, complications,
transfusions, and LOS were higher compared with
[8_TD$DIFF]
what
observed in patients with intermediate- and high-risk PCa
treated at our institution
[17]. Among patients with
nonmetastatic PCa treated at our center, for example, only
6.2% and 14.8% experienced postoperative complications and
blood transfusions, respectively. Similarly, we observed
substantially shorter median LOS (8 d) compared with the
metastatic scenario
[17] .Consequently, RP in oligometastatic
[(Fig._1)TD$FIG]
Fig. 1 – Kaplan-Meier analyses assessing the time from surgery to clinical progression (a) and cancer-specific mortality (b) in patients with
[6_TD$DIFF]
oligometastatic prostate cancer treated with radical prostatectomy.
CSM = cancer-specific mortality.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 8 9 – 2 9 2
291
















