
role of local treatment in oligometastatic patients; however,
the absence of predefined inclusion criteria, the lack of
details on the numbers and sites of metastases, and the
relatively short follow-up limited the generalizability of
their findings. Our study aimed to assess perioperative and
oncologic outcomes of RP in a selected cohort of patients
with bone metastases with a minimum follow-up of 5 yr.
After ethics committee approval, we retrospectively
evaluated 11 patients with oligometastatic PCa treated with
open RP and extended nodal dissection between 2006 and
2011 at a single high-volume center. The decision to
perform RP was left to the clinical judgment of the treating
physician after discussion with the patient regarding the
potential benefits and side effects of this procedure. All
patients signed informed consent. Oligometastatic disease
was defined as five or fewer lesions at bone scan with or
without suspicious pelvic or retroperitoneal nodal involve-
ment at preoperative imaging
[14] .All patients were
evaluated with abdominal computed tomography (CT)
and technetium Tc 99m bone scans before surgery. Targeted
CT (
n
= 7) and magnetic resonance imaging (MRI;
n
= 4)
were performed to confirm the results of bone scan. Patients
were considered to be affected by metastatic PCa if targeted
CT and/or MRI confirmed a positive bone scan. Five patients
(45%) underwent histologic confirmation of bone metasta-
ses. Additional cancer therapies were considered based on
patients’ and physicians’ preferences. Preoperative, patho-
logic, and follow-up data were available for all patients.
Operative time, blood loss, transfusions, 30-d complications
stratified according to the Clavien-Dindo classification,
length of stay (LOS), readmission, use of additional cancer
therapies, clinical progression, and cancer-specific mortali-
ty (CSM) were evaluated. Follow-up visits, physician
correspondence, and death certificates were used to
identify vital status and cause of death. Kaplan-Meier
analyses assessed time from RP to clinical progression and
CSM. All statistical analyses were performed using the R
statistical package (R Foundation for Statistical Computing,
Vienna, Austria).
Median age at surgery was 72 yr. The Charlson
comorbidity index was 0 in 73% of the patients
( Table 1).
Five patients (45%) had three or more bone metastases, and
two patients (18%) received neoadjuvant androgen depri-
vation therapy (ADT). Six patients had cN1 disease at
preoperative imaging. Median operative time was 170 min
(95% confidence interval [CI], 140–390 min), median blood
loss was 750 ml (95% CI, 550–850 ml), and median LOS was
13 d (95% CI, 7–21 d)
( Table 2 ). Two patients (18%; 95% CI, 1–
45%) experienced grade 3 complications in the postopera-
tive period, and eight patients (73%; 95% CI, 41–95%)
received transfusions. One patient (95% CI, 5–40%) needed
reintervention after surgery for anastomotic leakage. The
median number of nodes removed was 27. All patients
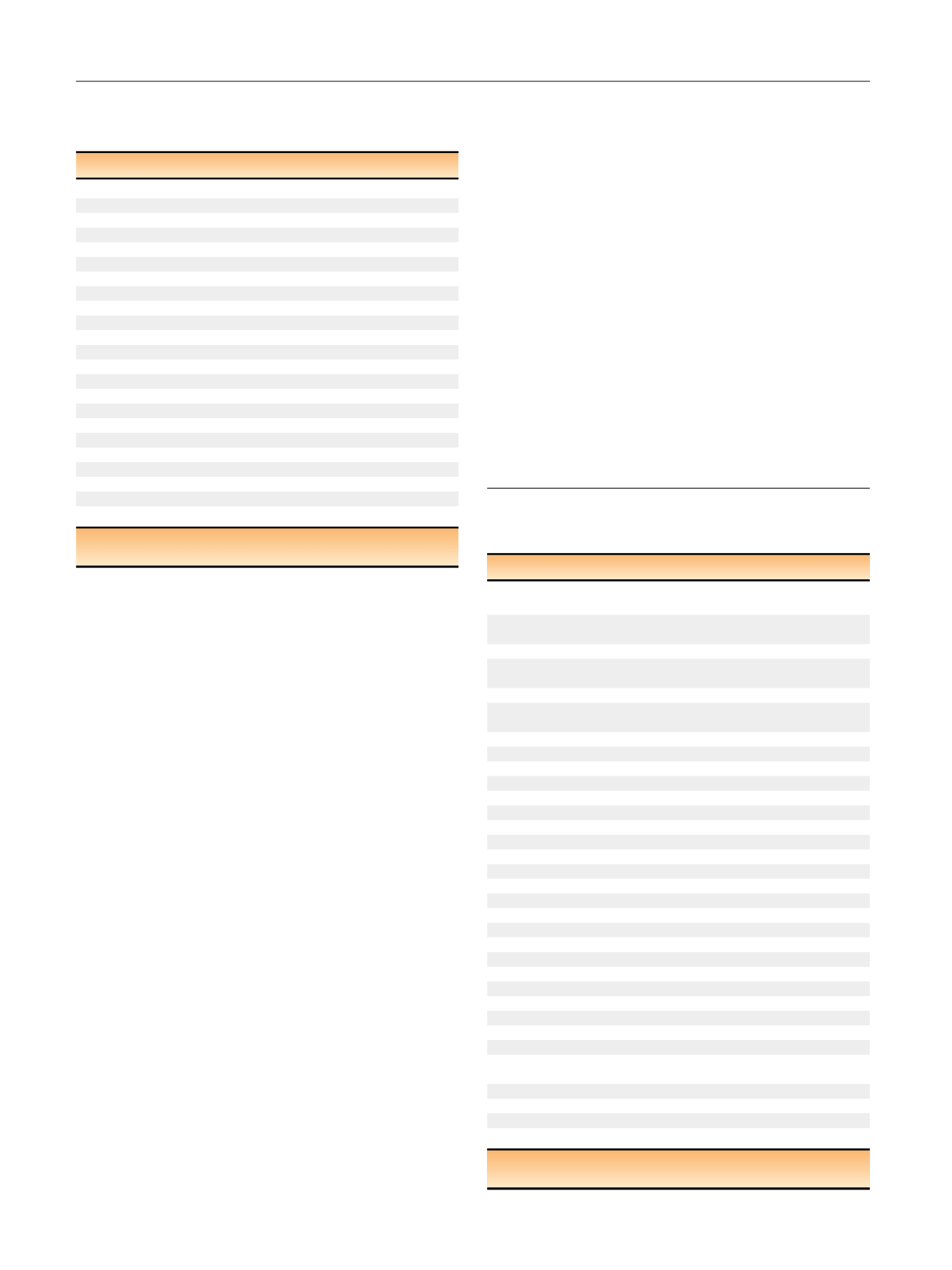
Table 1 – Preoperative characteristics of patients with
oligometastatic prostate cancer treated with radical
prostatectomy included in the study
Characteristic
Result
Age at surgery, yr, median (IQR)
72 (64–77)
BMI, kg/m
2
, median (IQR)
26.1 (22.8–27.8)
Charlson comorbidity index,
n
(%)
0
8 (72.7)
1
3 (27.3)
Prostate volume, ml, median (IQR)
32.5 (24.7–62.0)
Total PSA at diagnosis, ng/ml, median (IQR)
11.4 (5.7–22.5)
Clinical tumor stage,
n
(%)
cT1
3 (27)
cT2
5 (46)
cT3
3 (27)
Clinical nodal stage,
n
(%)
cN0
5 (45)
cN1
6 (55)
Biopsy Gleason score,
n
(%)
6
1 (9)
7
3 (27)
8–10
7 (64)
Neoadjuvant ADT,
n
(%)
2 (18)
No. of bone metastases,
n
(%)
1
2 (18)
2
4 (36)
3
5 (46)
ADT = androgen deprivation therapy; BMI = body mass index;
IQR = interquartile range; PSA = prostate-specific antigen.
Table 2 – Intraoperative, postoperative, and pathologic
characteristics of data of patients with oligometastatic prostate
cancer treated with radical prostatectomy included in the study
Characteristic
Result
Operative time, min, median (IQR),
95% CI
170 (160–380), 140–390
Intraoperative blood loss, ml,
median (IQR), 95% CI
750 (600–850), 550–850
Perioperative transfusions,
n
(%), 95% CI
8 (73), 41–95
Hospital length of stay, d, median (IQR),
95% CI
13 (7–19), 7–21
Postoperative complications,
n
(%), 95% CI
6 (54), 20–88
Postoperative complications according
to Clavien-Dindo,
n
(%)
Grade 1
2 (18)
Grade 2
2 (18)
Grade 3a
1 (9)
Grade 3b
1 (9)
Grade 4
0 (0)
Grade 5
0 (0)
Reoperation,
n
(%), 95% CI
1 (9), 5–40
Readmission,
n
(%), 95% CI
0 (0), NA
90-day continence,
n
(%
) * , 95% CI
3 (27), 5–58
Pathologic stage,
n
(%)
pT2c
1 (9)
pT3a
1 (9)
pT3b
7 (64)
pT4
2 (18)
pN1
10 (91)
Pathological Gleason score,
n
(%)
6
0 (0)
7
2 (18)
8-10
9 (82)
Positive surgical margins,
n
(%), 95% CI
8 (73), 41–95
No. of node removed, median (IQR)
27 (23–42)
No. of positive nodes, median (IQR)
4 (1–23)
Histologic confirmation of bone
metastases,
n
(%)
5 (45)
Adjuvant hormonal therapy,
n
(%)
10 (91)
Adjuvant radiotherapy,
n
(%)
7 (64)
Salvage radiotherapy at 7-yr follow-up, (%)
11.1
Follow-up, mo, median (IQR), 95% CI
63 (48–77), 48–77
CI = confidence interval; IQR = interquartile range; NA = not available.
*
Defined as the use of no pads.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 8 9 – 2 9 2
290
















