
EVL. Our aim was to specifically measure and assess the
independent impact of EVL on renal function at 3–12 mo
after surgery using our large PN database.
We retrospectively reviewed our institutional review
board-approved institutional robotic PN database to
identify predictors of glomerular filtration rate (GFR)
preservation (GFR-P). Six surgeons, all fellowship trained
or with 1 yr staff experience, were included in the study.
Baseline characteristics were captured by a chart review.
Covariates that may influence the rates of GFR-P were
selected a priori: age, sex, race, preoperative hypertension
or diabetes, body mass index (kg/m
2
[16_TD$DIFF]
), preoperative GFR,
RENAL score (4–6: low; 7–9: moderate; 10–12: high),
tumor diameter, warm ischemia time, EVL (log scale), and
Clavien complication grade (0; 1–2; 3). In all cases, tumors
were excised rather than enucleated, and a base suture layer
was run followed by a horizontal mattress cortical
renorrhaphy. Creatinine was measured preoperatively
within 1 mo of PN and again at 3–12 mo postoperatively,
allowing for estimation of GFR using the MDRD formula.
GFR-P was defined as 100 max GFR at 3–12 mo/
preoperative GFR. This time period for GFR was chosen
given that its decline stabilizes during this interval
(Supplementary Fig. 1)
[6] .EVL was calculated using
existing pathologic measurements as the difference be-
tween specimen and tumor volume, which amounts to the
rim of healthy excised parenchyma
[7]. This variable was
assessed with ladder plots, and log transformed to achieve a
normal distribution and a linear relationship with the
dependent variable. Univariate (UV) and multivariate (MV)
linear regressions were run to analyze the effect of
contributing covariates on GFR-P. In the linear marginal
effect model, a one-unit increase in the regressor
X
k
(log
EVL) produces an expected instantaneous rate of change in
Y
(GFR-P) of
b
units. All other independent variables are
adjusted for using their population-averaged predicted
values. Log terms were converted to nonlog terms using the
following formula:
D
Y
=
b
ln([
p
% + 100]/100).
The linear relationship between predictor and outcome
variables and the homoscedasticity and normality of resi-
duals was verified, and collinearity was tested. All statistical
testing was two sided, and a
p
value of
<
0.05 was considered
statistically significant. STATA 13 software (STATA, College
Station, TX, USA) was used for all statistical analyses.
A total of 647 patients with bilateral kidneys who
underwent robotic PN between 2006 and 2016 had GFR
data at 3–12 mo.
Table 1displays the baseline character-
istics of the study population. Our median EVL of 14.7 cm
3
(or log EVL of 2.69 cm
3
) was associated with a global GFR-P
of 90% at a median follow-up of 6 mo. On UV models
(Supplementary Table 1), significant associations with GFR-
P included preoperative GFR (
b
= –0.10,
p
= 0.002), tumor
diameter (
b
= –1.11,
p
= 0.007), warm ischemia time (con-
tinuous,
b
= –0.25,
p
= 0.005), and log EVL (
b
= –2.47,
p
<
0.001). On MV models, preoperative GFR (
b
= –0.14,
p
<
0.001), male sex (
b
= 4.08,
p
= 0.009), and log EVL
(
b
= –2.12,
p
= 0.005) were the only significant predictors.
In a high-volume single-center robotic PN cohort, we
have shown that EVL is the most important surgeon-
dependent factor associated with renal function at 3–12 mo
when standardized reconstructive techniques are
employed. Ischemia time and tumor complexity do not
have a significant association with GFR-P in our study,
either as independent or interaction variables. This would
suggest that, even for complex tumors, sacrificing ischemia
time in order to maximize the precision of tumor excision is
likely to benefit long-term renal function.
Our data are consistent with prior studies by Zargar et al
[7]and Kotamarti et al
[3], which demonstrated that EVL
was associated with postoperative ipsilateral renal function
on mercapto-acetyltriglycine
[18_TD$DIFF]
renal scan and chronic kidney
disease (CKD) upstaging, respectively. EVL is a heavily right-
skewed variable, which may explain why a linear relation-
ship with GFR-P is not always shown
[8]. However, after
logarithmic transformation, a statistically significant in-
verse linear relationship becomes readily apparent (Sup-
plementary Fig. 2). Given the complexity of factors
influencing GFR-P, it is unsurprising to see dispersion in
the scatterplot distribution of this UV relationship. Howev-
er, within the framework of our MV models, we found a
robust relationship between log EVL and GFR-P
( Fig. 1 ).
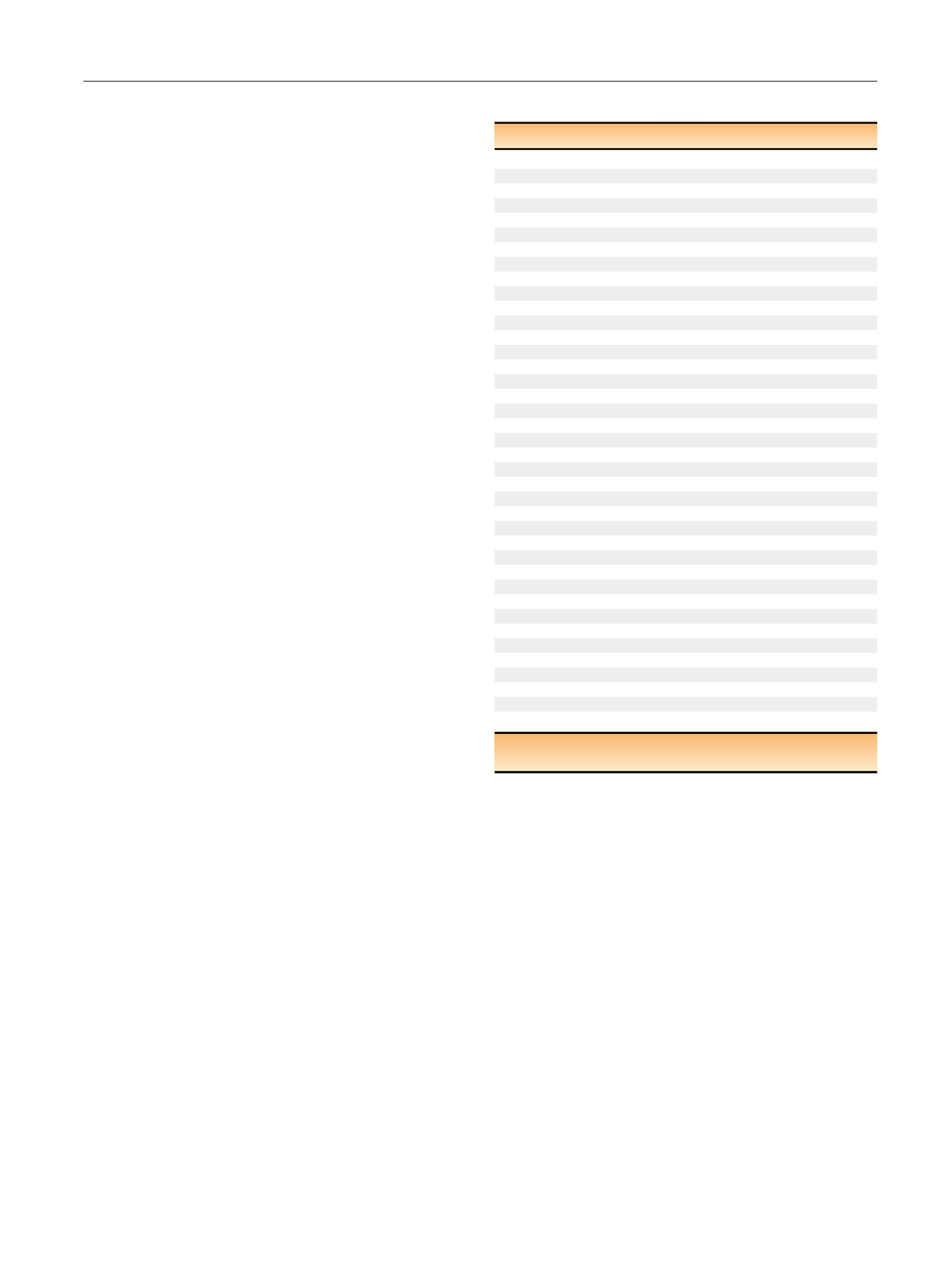
Table 1 – Patient, tumor, and surgical characteristics
Variables
Age category (%)
19.2
<
50
46.4
50–64
34.4
65+
Race, white (%)
86.3
Sex, male (%)
61.2
HTN (%)
56.7
Diabetes (%)
22.7
BMI, kg/m
2
(%)
19.0
<
25
34.6
25–29
24.9
30–34
21.5
35+
Preoperative GFR (med, IQR)
84.8 (69.0–97.7)
cT stage (%)
T1a
[4_TD$DIFF]
65.5
T1b
[5_TD$DIFF]
30.3
cT2+
[6_TD$DIFF]
4.2
RENAL score (%)
[2_TD$DIFF]
Low (4–6)
[7_TD$DIFF]
32.8
Moderate (7–9)
[8_TD$DIFF]
51.3
High (10+)
[9_TD$DIFF]
15.9
Warm ischemia time, min (med, IQR)
22 (16–27)
Tumor diameter, cm, max dimension (med, IQR)
3 (2.1–4.4)
Tumor volume, cm
3
[1_TD$DIFF]
(med, IQR)
9.5 (
[10_TD$DIFF]
3.5–27.7)
Specimen volume, cm
3
(med, IQR)
28.0 (13.0–59.4)
Excisional volume loss, cm
3
[11_TD$DIFF]
(med, IQR)
14.7 (
[12_TD$DIFF]
6.5–28.8)
No. of tumors excised (%)
1
95.7
2+
4.3
Renal cell carcinoma (%)
86.4
Positive margins (%)
5.6
Clavien category
0
80.1
1–2
14.0
3+
5.9
GFR f/u, mo (med, IQR)
6.0 (
[13_TD$DIFF]
4.5–9.9)
Postoperative GFR (med, IQR)
75.0 (
[14_TD$DIFF]
60.1–90.0)
% GFR preservation (med, IQR)
90.0 (
[15_TD$DIFF]
80.3–100)
BMI = body mass index; f/u = follow-up; GFR = glomerular filtration rate;
HTN = hypertension; IQR = interquartile range; med = median.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 1 6 8 – 1 7 0
169
















