
unaccounted for. Moreover, given that the database
only captures patients per in-hospital admission, it was
not possible to track a patient’s previous diagnostic
and treatment workup, similar to previously published
work
[9]. In that regard, hospital-admitted patients may
not be representative of the entire metastatic renal cell
carcinoma population. Finally, we could not ascertain
if patients underwent a metastasectomy for palliative
reasons.
Taken together, our study emphasizes that postoperative
complications are not insignificant, regardless of the type of
hospital or the number of cancer cases the facility treats
annually. As the role of metastasectomy will be better
defined in the future for the treatment of mRCC, its
utilization rate may subsequently increase, and with that
further improvement in patient selection, surgical tech-
nique, and postoperative care is required. The current
findings may aid in the preoperative counseling of patients
undergoing a metastasectomy.
Author contributions:
Christian P. Meyer had full access to all the data in
the study and takes responsibility for the integrity of the data and the
accuracy of the data analysis.
Study concept and design:
Meyer, Sun, Choueiri.
Acquisition of data:
Meyer, Trinh, Sun.
Analysis and interpretation of data:
Meyer, Sun, Karam, Leow, Choueiri.
Drafting of the manuscript:
Meyer, Karam, Leow, Sun, Choueiri.
Critical revision of the manuscript for important intellectual content:
de
Velasco, Chang, Pal, Trinh.
Statistical analysis:
Meyer, Sun.
Obtaining funding:
Choueiri, Trinh.
Administrative, technical, or material support:
Meyer, Sun, Karam, Leow,
de Velasco, Pal, Chang, Trinh, Choueiri.
Supervision:
Sun, Choueiri.
Other:
None.
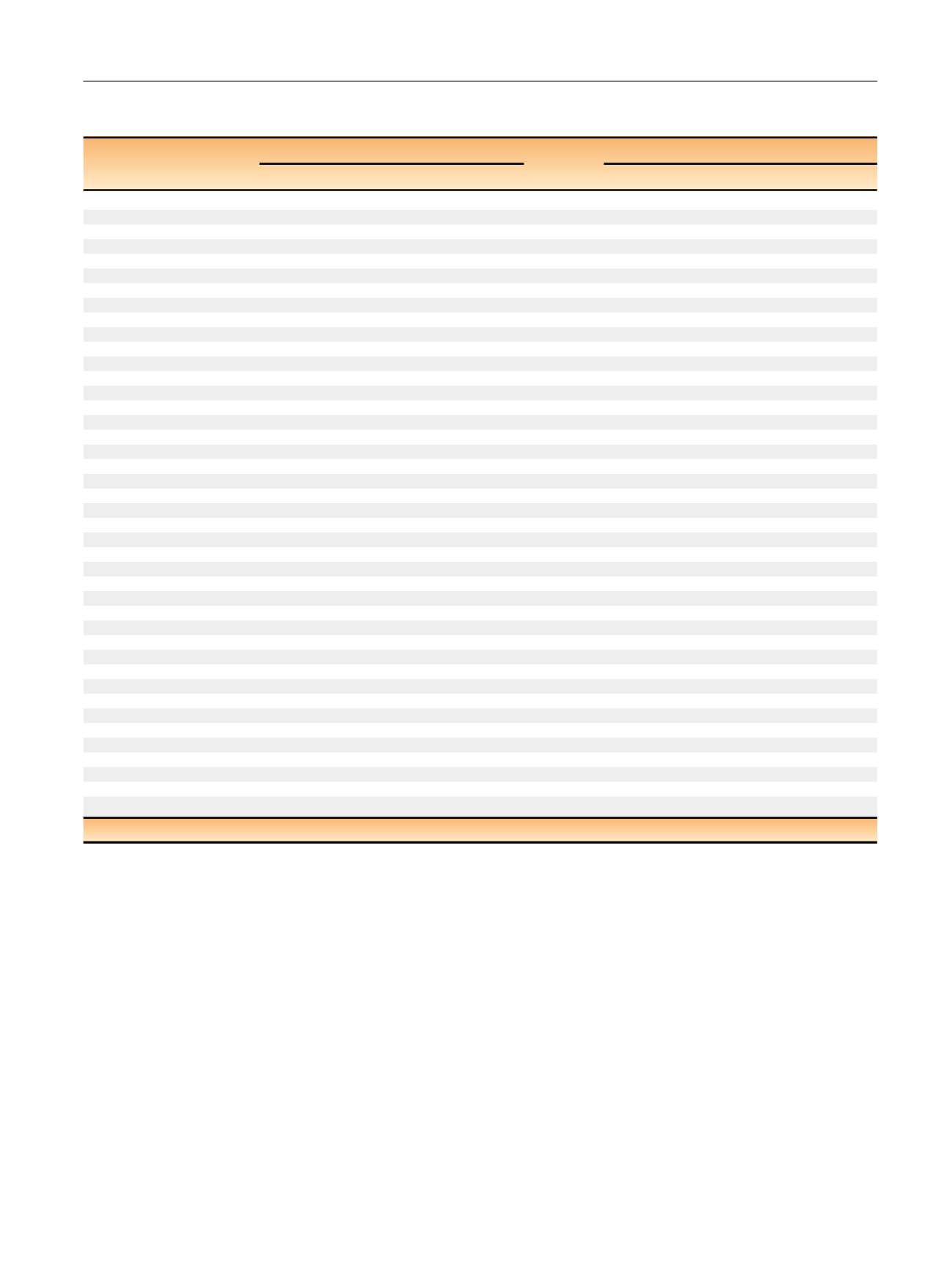
Table 1 – Univariable analysis of covariates associated with overall and major complications after metastasectomy (
n
= 1102) for RCC, NIS
2000–2011.
Overall complications
Major Clavien (III–IV)
OR
95% CI
p
OR
95% CI
p
Years
<
2006
Ref.
Ref.
2006
1.27
0.99–1.61
0.054
1.09
0.83–1.44
0.53
Age
1.02
1.01–1.03
0.001
1.01
1.01–1.03
0.04
Gender
Male
Ref.
Ref.
Female
1.08
0.83–1.39
0.56
0.79
0.59–1.07
0.13
Charlson–Deyo score
0
Ref.
Ref.
1
1.09
0.82–1.44
[1_TD$DIFF]
0.56
1.12
0.86–1.65
0.30
2
1.48
0.99–2.19
[2_TD$DIFF]
0.06
2.41
1.60–3.62
<
0.001
Annual hospital volume
Low
Ref.
Ref.
High
0.91
0.72–1.15
0.43
0.86
0.65–1.13
0.26
Race
White
Ref.
Ref.
Black
1.64
0.92–2.90
0.097
1.31
0.69–2.46
0.42
Hispanic
0.97
0.60–1.57
0.91
0.97
0.54–1.74
0.97
Other
1.31
0.68–2.52
0.42
1.11
0.51–2.40
0.79
Unknown
1.06
0.78–1.48
0.71
1.01
0.71–1.43
0.95
Payor
Medicare
Ref.
Ref.
Medicaid
0.82
0.77–1.14
0.48
0.73
0.37–1.43
0.35
Private/self-pay
0.85
0.66–1.08
0.19
0.68
0.51–0.92
0.01
Other
0.70
0.36–1.37
0.30
0.66
0.30–1.44
0.66
Hospital location
Rural
Ref.
Ref.
Urban
1.22
0.69–2.17
0.50
1.23
0.66–2.29
0.52
Hospital size
Small
Ref.
Ref.
Intermediate
1.39
0.84–2.29
0.21
1.59
0.83–3.04
0.16
Large
1.38
0.89–2.15
0.15
1.45
0.80–2.62
0.22
Hospital status
Nonteaching
Ref.
Ref.
Teaching
1.03
0.79–1.34
0.81
1.02
0.76–1.37
0.91
Metastatic location
Any other
Ref.
Ref.
Liver
2.59
1.84–3.62
<
0.001
1.34
0.94–1.91
0.11
Lung
0.63
0.50–0.81
<
0.001
0.99
0.76–1.31
0.97
Adrenal
0.63
0.38–1.03
0.066
0.86
0.49–1.51
0.59
Bone
0.99
0.76–1.30
0.98
0.80
0.59–1.10
0.17
Lymph node
1.20
0.76–1.88
0.44
1.24
0.76–2.04
0.39
NIS = National Inpatient Sample; RCC = renal cell carcinoma; Ref. = reference.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 1 7 1 – 1 7 4
173
















