
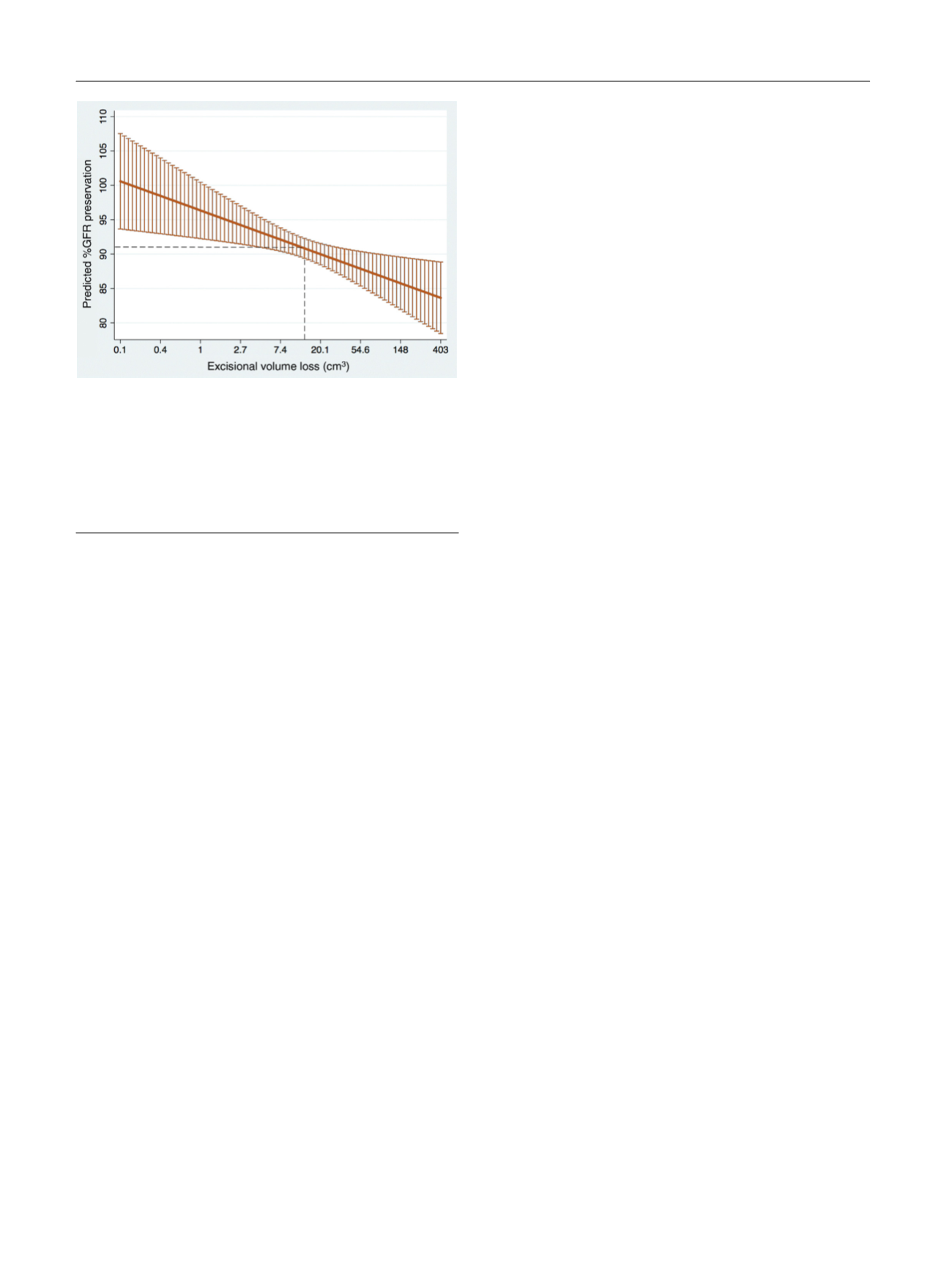
To make the clinical context more apparent, let us
presume a scenario whereby EVL increases by 400% but all
other factors affecting GFR-P remain constant. Taking a
standard 3-cm 50% endophytic tumor, this would mean
increasing the margin from 5 mm to 2 cm. In nonlog terms,
this corresponds to a predicted loss of GFR-P of 3.4%. Given
this relatively small but significant effect, attempts to limit
EVL appear to be most relevant for patients with CKD or CKD
risk factors
[9] .Indeed, opportunities for improvement
exist, as EVL has been shown to be sensitive to influences of
factors including bleeding, surgeon experience, and ap-
proach
[10] .Our study is the largest to date examining the functional
effect of EVL and has the advantages of accounting for
ischemia time, employing standardized robotic technique,
and including a defined timeframe during which GFR decline
plateaus. By specifically measuring EVL and accounting for
other modifiable and confounding factors, we have shown
that improved excisional precision can significantly mitigate
the iatrogenic effects of tumor excision on renal function
months after PN, which is especially critical when nephron
preservation is of utmost importance.
Study limitations include the following: (1) retrospective
design, (2) error of volumetric estimates based on ellipsoid
assumptions, and (3) inability to account for percent
volume loss or total parenchymal volume loss.
Author contributions:
Jihad H. Kaouk had full access to all the data in the
study and takes responsibility for the integrity of the data and the
accuracy of the data analysis.
Study concept and design:
Dagenais, Maurice, Kaouk.
Acquisition of data:
Dagenais, Maurice, Mouracade, Kara, Malkoc.
Analysis and interpretation of data:
Dagenais, Maurice.
Drafting of the manuscript:
Dagenais.
Critical revision of the manuscript for important intellectual content:
Dagenais, Maurice, Mouracade, Kara, Kaouk.
Statistical analysis:
Dagenais, Maurice.
Obtaining funding:
None.
Administrative, technical, or material support:
Kaouk.
Supervision:
Kaouk.
Other:
None.
Financial disclosures:
Jihad H. Kaouk certifies that all conflicts of interest,
including specific financial interests and relationships and affiliations
relevant to the subject matter or materials discussed in the manuscript
(eg, employment/affiliation, grants or funding, consultancies, honoraria,
stock ownership or options, expert testimony, royalties, or patents filed,
received, or pending), are the following: Endocare, Inc.—J.H. Kaouk
(consultant).
Funding/Support and role of the sponsor:
None.
Appendix A. Supplementary data
Supplementary data associated with this article can be
found, in the online version, at
http://dx.doi.org/10.1016/j. eururo.2017.02.004 .References
[1]
Mir MC, Ercole C, Takagi T, et al. Decline in renal function after partial nephrectomy: etiology and prevention. J Urol 2015;193: 1889–98.[2]
Rod X, Peyronnet B, Seisen T, et al. Impact of ischaemia time on renal function after partial nephrectomy: a systematic review. BJU Int 2016;118:692–705.[3]
Kotamarti S, Rothberg MB, Danzig MR, et al. Increasing volume of non-neoplastic parenchyma in partial nephrectomy specimens is associated with chronic kidney disease upstaging. Clin Genitourin Cancer 2015;13:239–43.[4]
Bahler CD, Sundaram CP. Effect of renal reconstruction on renal function after partial nephrectomy. J Endourol 2016;30(Suppl 1):S37–41.[5]
Takagi T, Mir MC, Campbell RA, et al. Predictors of precision of excision and reconstruction in partial nephrectomy. J Urol 2014;192:30–5.[6]
Porpiglia F, Fiori C, Bertolo R, et al. The effects of warm ischaemia time on renal function after laparoscopic partial nephrectomy in patients with normal contralateral kidney. World J Urol 2012;30:257–83.[7]
Zargar H, Akca O, Autorino R, et al. Ipsilateral renal function preservation after robot-assisted partial nephrectomy (RAPN): an objective analysis using mercapto-acetyltriglycine (MAG3) renal scan data and volumetric assessment. BJU Int 2015;115:787–95.[8]
Golan S, Patel AR, Eggener SE, Shalhav AL. The volume of nonneo- plastic parenchyma in a minimally invasive partial nephrectomy specimen: predictive factors and impact on renal function. J Endourol 2014;28:196–200.[9]
Satasivam P, Reeves F, Rao K, et al. Patients with medical risk factors for chronic kidney disease are at increased risk of renal impairment despite the use of nephron-sparing surgery. BJU Int 2015;116: 590–5.[10]
Maurice MJ, Ramirez D, Malkoc E, et al. Predictors of excisional volume loss in partial nephrectomy: is there still room for im- provement? Eur Urol 2016;70:413–5.[(Fig._1)TD$FIG]
Fig. 1 – Marginal effect of excisional volume loss on GFR preservation.
Each value of
x
(EVL, log scale) yields a predicted value of
y
(%GFR
preservation) while controlling for age, sex, race, diabetes mellitus,
hypertension, body mass index, preoperative GFR, RENAL score,
maximum tumor diameter, Clavien complication grade, and ischemia
time. Confidence intervals set to 95%; %GFR preservation is calculated
as maximum GFR at 3–12 mo/preoperative GFR * 100. Dashed lines
mark the median value of EVL of 14.7 cm
3
. EVL = excisional volume loss;
GFR = glomerular filtration rate.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 1 6 8 – 1 7 0
170
















