
abstracted (
n
= 45 279). Patients who underwent a metas-
tasectomy were identified using concomitant codes of the
site of metastases, as well as the code for the procedure
corresponding to organ-specific resection, as described
previously
[2] .The main outcomes of interest were overall
and major complications (Clavien grade III–IV). Covariates
consisted of metastatic sites (lung, liver, bone, adrenal
gland, and lymph node), time of surgery (target vs non-
target therapy era [ 2006 vs
<
2006]) patient age, sex, race/
ethnicity, insurance status, Charlson Comorbidity Index
(CCI), as well as hospital location, academic status, hospital
size, and annual caseload. Univariable logistic regression
models assessed the association of covariates with overall
and major complications. All results were weighted to
reflect national estimates. A two-sided
p
value of
<
0.05 was
considered to be statistically significant. This study was
reviewed and deemed exempt from approval by the
Brigham and Women’s Institutional Review Board.
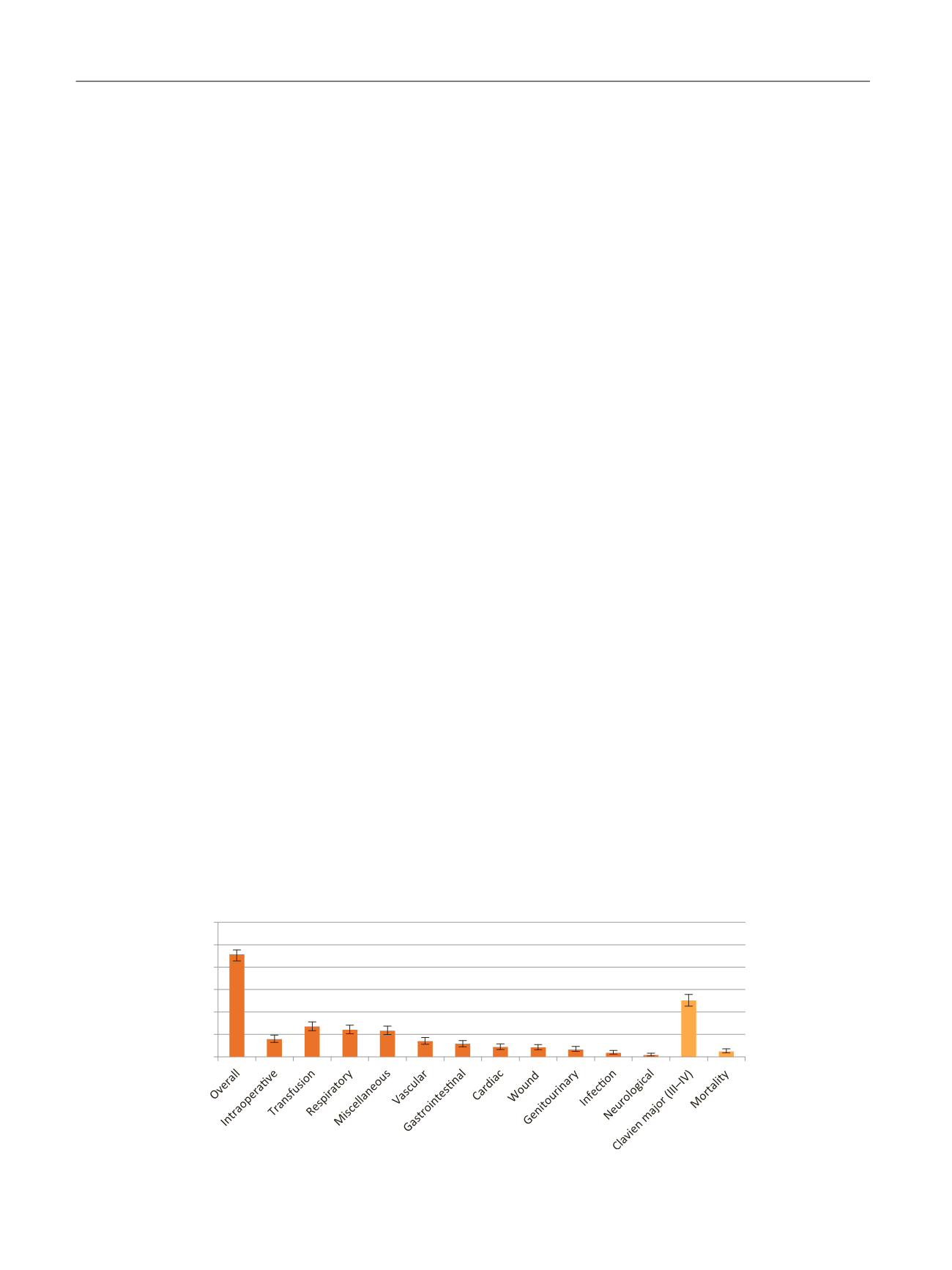
Overall, 1102 metastasectomies were identified (Sup-
plementary Table 1). Most common metastatic sites were
the lungs (51.8%), bone (29%), and liver (18.6%, Supplemen-
tary Fig. 1). Metastasectomy was predominantly performed
for lung (43.5%), bone (27.1%), and liver (16.1%) lesions.
Intraoperative complications occurred in 7.9% of patients.
The overall complication rate was 45.7%. The most frequent
complication types were of respiratory (12.0%) nature.
Major complications (Clavien III–IV) occurred in 25.1%. In-
hospital mortality rate (Clavien V) was 2.4%
( Fig. 1).
Univariable logistic regression analysis identified in-
creasing age (odds ratio [OR]: 1.02, 95% confidence interval
[CI]: 1.01–1.03,
p
= 0.001), and hepatic (OR 2.59, 95% CI
1.84–3.62,
p
<
0.001) and pulmonary metastasis (OR 0.63,
95% CI 0.50-0.81, p
<
0.001), both compared with any other
site, as independent predictors of overall complications
( Table 1). Predictors of major complications were a high
comorbidity burden (CCI 2; OR: 2.41, 95% CI: 1.60–3.62,
p
<
0.001) and private insurance (OR: 0.68, 95% CI: 0.51–
0.92,
p
= 0.01).
Our study provides several important findings regarding
short-term outcomes following metastasectomy for
mRCC. Consistent with previous reports
[1,3] ,major
complications (Clavien III–IV) were recorded in one-fourth
of metastasectomy patients. Overall, in-hospital mortality
after a metastasectomy was 2.4% (
n
= 27), of which the
majority underwent lung (
n
= 11) or bone (
n
= 9) resections.
The rate of perioperative mortality following metastasect-
omy was comparable with that in previous reports
(0.9–2.3%)
[4,5].
In the current study, patients in the target therapy era
(
>
2006) did not experience a higher likelihood of in-
hospital complications after metastasectomy. While it has
previously been observed in the context of cytoreductive
nephrectomy that presurgical systemic therapy is associat-
ed with higher rates of 90-d complications,
>
1 complica-
tion, and wound complications
[6], the association with
systemic therapies could not be ascertained for metasta-
sectomies with the data at hand.
Unsurprisingly, a higher comorbidity score was signifi-
cantly associated with major complications, similar to
previous findings
[7]. We also established a significantly
higher likelihood of overall complications among liver
resections. This is likely due to the fact that visceral
metastases have more detrimental effects on survival and
are most difficult to make amenable to successful therapy.
Contrary to synchronous hepatic resection for direct
invasion or metastatic disease during nephrectomy, we
could not establish a higher likelihood for Clavien grade III–
IV complications in hepatic resections
[8] .It is possible that
the significantly lower association of covariates with overall
complications in pulmonary resections compared with any
other site is a consequence of a more routine surgical
approach in this most common metastatic location.
Several limitations are applicable. First, the validity of
the Clavien classification using International Classification
of Diseases, ninth revision, diagnostic codes has not been
assessed, despite its use in other population-based reports
[7] .Although the bias of procedural misclassifications cannot be
ruled out entirely, we relied on the previous methodology,
which demonstrated robust outcomes
[9] .Second, since
the data capture only in-hospital events, 90-d morbidity
could not be assessed. Third, the retrospective nature
of the study is associated with a selection bias; unmea-
sured confounders such as the number of metastases
operated, type of surgery, synchronous or metachronous
metastasis, performance status at surgery, or risk group
classification; and other residual errors that are mostly
[(Fig._1)TD$FIG]
45.7
7.9
13.5 12 11.6
6.9 5.8 4.3 4.2 3.3 1.8 0.8
25.1
2.4
60
50
40
30
20
10
0
Fig. 1 – National estimated overall complications/outcomes of metastasectomies for RCC (in %), NIS 2000–2011. Bars represent 95% confidence intervals.
NIS = National Inpatient Sample; RCC = renal cell carcinoma.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 1 7 1 – 1 7 4
172
















