
multiple calyceal stones (85% for mPNL vs 70% for standard
PNL,
p
<
0.05). The duration of the procedure was longer in
the mPNL group for all stone types (all
p
<
0.05;
Table 1).
The other RCT was a comparison of
m
PNL (4.8 Fr) and
standard PNL (30 Fr)
[28]. No benefit was found with respect
to ISFR (
p
= 1), although blood loss and procedure duration
were lower (
p
= 0.004 and 0.034, respectively) and hospital
stay was shorter (
p
= 0.001). Intrarenal pelvic pressure was
higher in the
m
PNL group (
p
<
0.0001;
Table 1).
3.4.
NRCSs
Six NRCSs were included, all of which were full-text articles.
One study compared five groups with successively increas-
ing PNL tract size (22, 24, 26, 28, and 30 Fr)
[21] .Blood loss
increased with the tract size (
p
<
0.05) but the procedure
duration did not significantly differ between the groups
( Table 2 ). Another study using the PNL Global Study database
of The Clinical Research Office of the Endourological Society
(CROES) reported data for four groups ( 18, 24–26, 27–30,
and 32 Fr)
[27] .The only relevant outcomes were blood
loss and blood transfusion rates, which significantly
increased with the tract size (
p
= 0.00016 and
<
0.0001).
Four comparative studies comprised two main comparator
groups (mPNL vs standard PNL). In one of the studies
[11] ,the control arm (30 Fr) was further divided into two groups:
patients who received a nephrostomy tube and patients who
did not (tubeless). SFR was lower in the mPNL group (14 Fr)
than in either of the standard PNL groups (tube
p
= 0.016 and
tubeless
p
= 0.009). Blood loss was lower than in the tube
standard PNL group (
p
= 0.021) but not the tubeless standard
PNL group (
p
= 0.041). Tubeless standard PNL was also
superior in terms of analgesic requirement, pain (VAS), and
duration of procedure and hospital stay
( Table 2). Xu et al
[26]compared 16 Fr mPNL with 24 Fr PNL, and observed
lower blood loss in the mPNL group (
p
= 0.015), although the
stones treated were also smaller. ISFR, complication rates,
procedure duration, and hospital stay did not differ
( Table 2 ).
Mishra et al
[24]compared mPNL (14–18 Fr) with standard
PNL (24–28 Fr), but interpretation of the results is obscured
by the use of different energy sources for stone fragmenta-
tion: laser in the mPNL group and pneumatic in the standard
PNL group
[24] .The study reported similar SFR (
p
= 0.49) and
analgesic requirement (
p
= 0.28), but lower blood loss
(
p
= 0.0098) and procedure duration (
p
= 0.0008), and
shorter hospital stay (
p
<
0.00001) in the mPNL group. A
greater proportion of procedures were tubeless in the mPNL
(78%) than in the standard PNL group (14%;
p
<
0.001). Knoll
et al
[22]compared mPNL (18 Fr) and standard PNL (26 Fr)
and found similar ISFR in both groups (
p
= 1.00). However,
stones were significantly larger in the standard PNL group
(
p
= 0.042). The study also revealed similar blood loss,
complication rates, procedure duration, and analgesic
requirements for both groups (all
p
>
0.05). However pain
scores (VAS) were lower (
p
= 0.048) and hospital stay was
shorter (
p
= 0.021) among mPNL patients. All mPNL proce-
dures were tubeless if uncomplicated and the patient was
rendered stone-free, otherwise a nephrostomy tube was
placed. All patients undergoing standard PNL received a
nephrostomy tube.
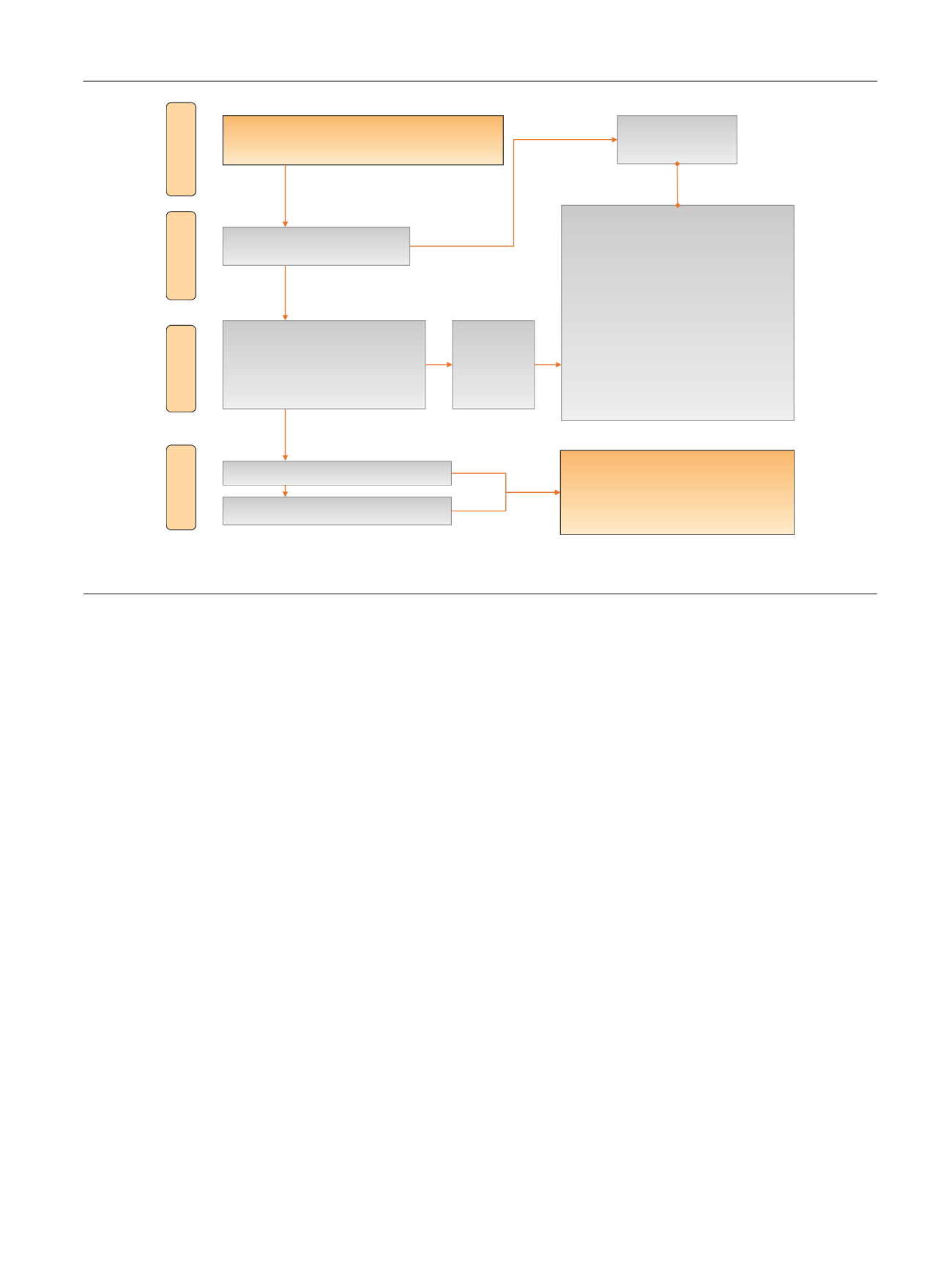
[(Fig._1)TD$FIG]
Records identified through database searching
(
n
= 2945)
Abstracts screened (
n
= 2945)
Excluded
(
n
= 222)
(
n
= 99)
(
n
= 123)
Abstracts assessed for eligibility
Total (
n
= 240)
Full-text articles (
n
= 112)
Conference abstracts (
n
= 128)
Full-text articles included (
n
= 13)
Screening
Included
Eligibility
Identification
Conference abstracts included (
n
= 5)
Records excluded
n
= 2705
Reasons for exclusion
• Language other than English
• Intervention not relevant
• Population unclear
• Basic science studies
• Participants in case series with
n
<2 0
• Cases <18 yr of age >10%
• Cases with anatomical anomalies >10%
• Cases treated bilaterally >10%
• Multiple tracts used in >10% of cases
• Data not in useable format
• Imaging studies
• Duplicate studies or duplicate data
Studies included in systematic review
Total (
n
= 18)
• 2 RCTs
• 6 NRCSs
• 10 case series
Fig. 1 – Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram showing the screening process for inclusion of
studies. RCT = randomized controlled trial; NRCS = non-randomized comparative study.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 2 0 – 2 3 5
223
















