
3.7.2.
Implications for practice
Our systematic review demonstrates that the use of
miniaturized PNL systems is effective. This was demon-
strated in most studies, including the first series published
by Jackman et al
[6]. The authors reported SFR of 85% in
children and 85% in adults for stones sized 12–15 mm. One
of the few studies showing inferiority for smaller instru-
ments was the series described by Giusti et al
[11]. However,
this study demonstrates the confusion caused by non-
standardized terminology, as the instruments used were
not dedicated for PNL but rigid ureteroscopes of small
diameters. The major disadvantage of small instruments is
that it is necessary to fragment stones into smaller pieces
that fit through the narrower sheaths, leading to longer
operating times compared to standard PNL, which allows
removal of large stone fragments with forceps and baskets.
Conversely, extraction of stone fragments seems to be
facilitated by modified Amplatz sheaths, as fragments can
be removed via vacuum suction, an effect that works best
for tracts sized 13–18 Fr
[41–43] .The idea behind downsizing PNL is based on the
assumption of lower morbidity than for conventional
PNL. However, there is still controversy regarding whether
miniaturization leads to such a benefit. Li et al
[44]investigated systemic responses to both standard and
mPNL by measuring acute-phase proteins, and found no
significant differences between the groups. In another
experimental approach, Traxer et al
[45]measured the
extent of damage to the renal parenchyma in pigs
undergoing placement of 11 Fr or 30 Fr nephrostomy tubes.
There were no detectable differences in fibrotic scar
volumes. The hypothesis of lower blood loss with minia-
turized tracts has only been confirmed in a few studies.
Mishra et al
[24]reported a slight but clinically significant
advantage for 18 Fr compared to 26 Fr access. However,
others could not confirm such a benefit
[22] .The observa-
tion in many series that the rate of tubeless procedures is
much higher than in conventional PNL series may support
the idea of lower intraoperative bleeding, if it is assumed
that a tubeless procedure is performed after uncomplicated
access and stone removal
[22,24]. In addition, a meta-
analysis of tubeless versus standard PNL procedures
[46]indicated that tubeless procedures led to shorter hospital
stay, less postoperative pain, and possible quicker recovery,
and may therefore contribute to lower morbidity in
miniaturized PNL. However, most patients with so-called
tubeless procedures received a double-J stent instead of a
nephrostomy tube. As stent-related discomfort is common,
this has to be taken into account and evaluated in future
studies. Sealants are used in tubeless procedures, but their
potential benefit remains controversial
[47,48]. Complica-
tion rates for mPNL according to the Clavien-Dindo
classification range from 11.9% to 37.7%
[49,50]. Most
complications in published series were of low grade, with
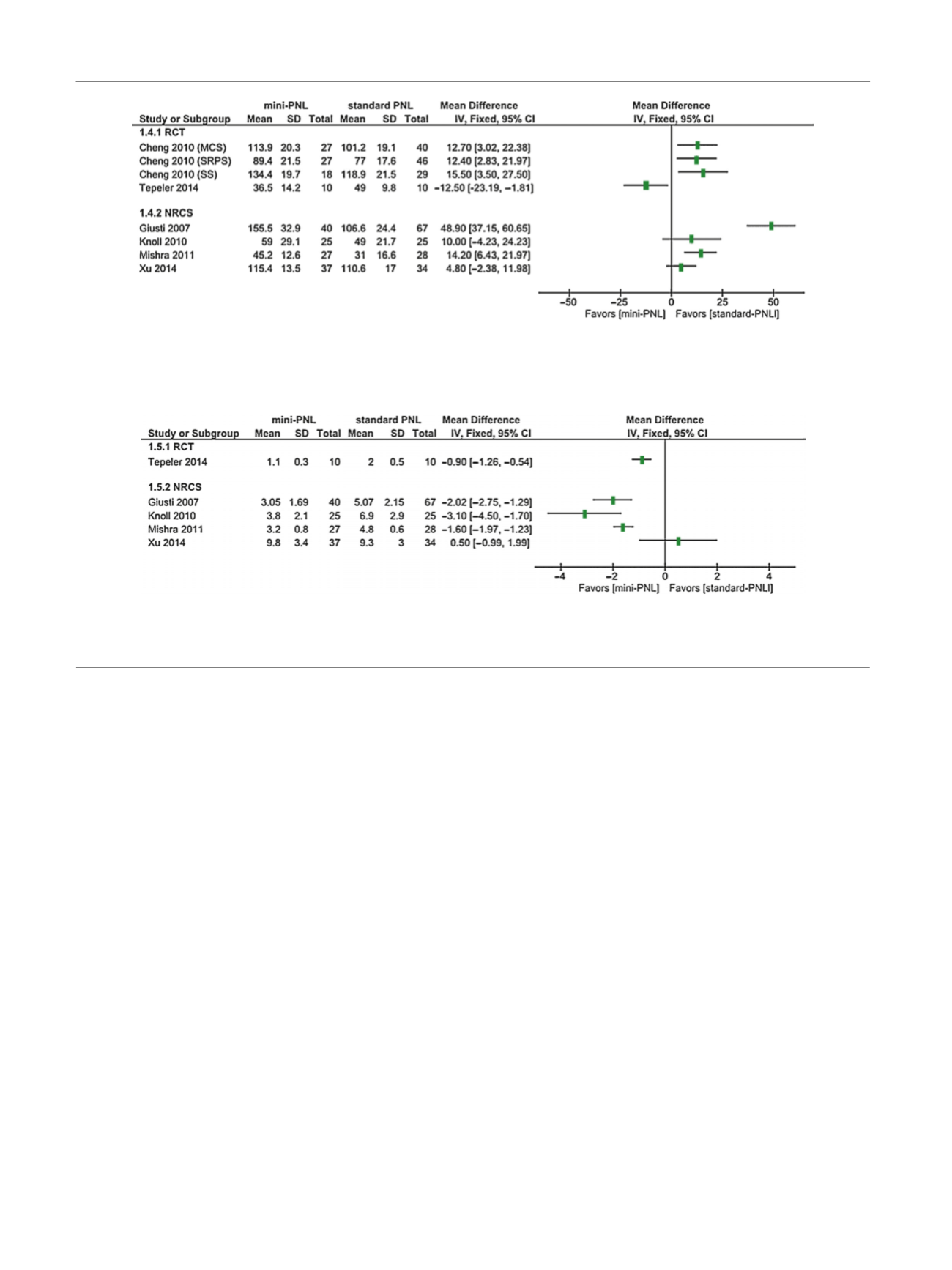
[(Fig._6)TD$FIG]
Fig. 6 – Forest plot showing the length of hospital stay (d) reported in randomized controlled trials (RCTs) and nonrandomized comparative studies
(NRCS). Reference numbers for studies are given in
Table 1 .PCNL = percutaneous nephrolithotomy; SD = standard deviation; CI = confidence interval;
IV = inverse variance.
[(Fig._5)TD$FIG]
Fig. 5 – Forest plot showing the duration of the procedure (min) reported in randomized controlled trials (RCTs) and nonrandomized comparative
studies (NRCS). Reference numbers for studies are given in
Table 1. PCNL = percutaneous nephrolithotomy; SD = standard deviation; CI = confidence
interval; IV = inverse variance.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 2 0 – 2 3 5
232
















