
 (
Table 1
)
(
Table 1
)
. D’Amico et al
[7]first proposed a risk group system
based on data from 1872 patients treated with RP or
radiotherapy (RT) with or without androgen deprivation
therapy. Groups were defined based on the incremental risk
of developing biochemical recurrence. Consequently, the
European Association of Urology
[8]and American Urologi-
cal Association adopted this risk scoring classification. The
Radiation Therapy Oncology Group also proposed a system
to predict overall and cancer-specific mortality in PCa
patients treated with radiation only
[9] .These grouping
systems were improved by continuous multivariate models
of risk such as nomograms and integrating standard
pathological variables such as number of biopsy cores
involved and the percentage of cores involved
[10,11]. Al-
though these refinements better discriminate disease risk
than the simpler operational definitions, their greatest
utility is in those with intermediate and high-risk disease.
The current National Comprehensive Cancer Network
guidelines
[12]implemented divided low-risk disease into
two classes: very-low and low-risk groups. Although the
definition of low-risk PCa disease is consistent with the
previously described, the very-low risk population includes
a subgroup of low-risk patients with the following
characteristics: clinical stage T1c, Gleason score 6, PSA
<
10 ng/ml,
<
3 biopsy cores with cancer,
50% PCa
involvement in any core, and PSA density
<
0,15 ng/ml/g,
which is based on criteria proposed by Epstein et al
[13]for
determining the optimal biopsy findings associated with
low-volume, low-grade cancer at RP. In a recent update of
the Epstein criteria, unilateral cancer has replaced 50% PCa
involvement in any core
[14] .3.2.
The new grade group grading system and its impact on
low-risk PCa
Consensus conferences of 2005 and 2014 modified the
Gleason grading system leading to the elimination of
Gleason scores 2–5 and set a more restrictive definition
of Gleason score 6
[15,16]. The major consequence of these
changes is a more favorable prognosis of patients diagnosed
with contemporary Gleason 6 compared with historical
patients
[17,18]. Therefore, a new grading system com-
posed of five grades where grade group 1 is equivalent to
contemporary Gleason score 6 has been developed by
Epstein and colleagues
[13]. Informing patients that they
have a potentially indolent-behaving cancer reflected in
grade group 1 has the potential to permit more rational and
less emotional decision-making
[19,20]. This system has
been recently adopted by the World Health Organization
[21,22], in the cancer protocol templates and 8th revision of
the TNM.
3.3.
Prospective trials evaluating the management of low-risk
PCa
The natural history of PCa and the impact of radical
treatment on survival and functional outcomes have been
investigated by several randomized trials
[23–25] .Of these,
only two analyzed outcomes of men with low-risk PCa
( Table 2)
[23,24]. Wilt et al
[23]reported data from the
Prostate Cancer Intervention versus Observation Trial
where 731 patients were randomly assigned between
1994 and 2002 to RP or observation with a median follow
up of 10 yr. Patients aged less than 75 yr were recruited
from multiple centers and had a clinical stage of T1–
T2NxM0 and PSA
<
50 ng/ml. At 12 yr, the cancer-specific
mortality rates were 4.4% versus 7.4% for patients treated
with RP versus patients observed, respectively (
p
= 0.09).
Considering 296 low-risk PCa patients, 148 were treated
with RP and 148 were observed. No differences were found
considering survival expectations, where patients treated
with RP or observation recorded both a 12-yr cancer-
specific mortality of 2.7% (
p
= 0.5).
These results should be interpreted within the limita-
tions of the study as the original power calculation was
based on the recruitment of 2000 cases, while it was
subsequently adjusted for the recruitment of 740 men and
results are therefore underpowered. Moreover, only 25% of
all men had a Gleason score of 7. Another limitation is
represented by the fact that despite eligibility criteria
including a 10-yr life expectancy and surgically curable
disease, almost half of patients died of other causes before
10 yr and only half treated with surgery had an organ-
confined disease.
Bill-Axelson et al
[24]reported on the Scandinavian
Prostate Cancer Group Study Number 4 where 695 men
with localized PCa were randomly assigned to RP or
observation. Patients were treated at 14 centers in Sweden,
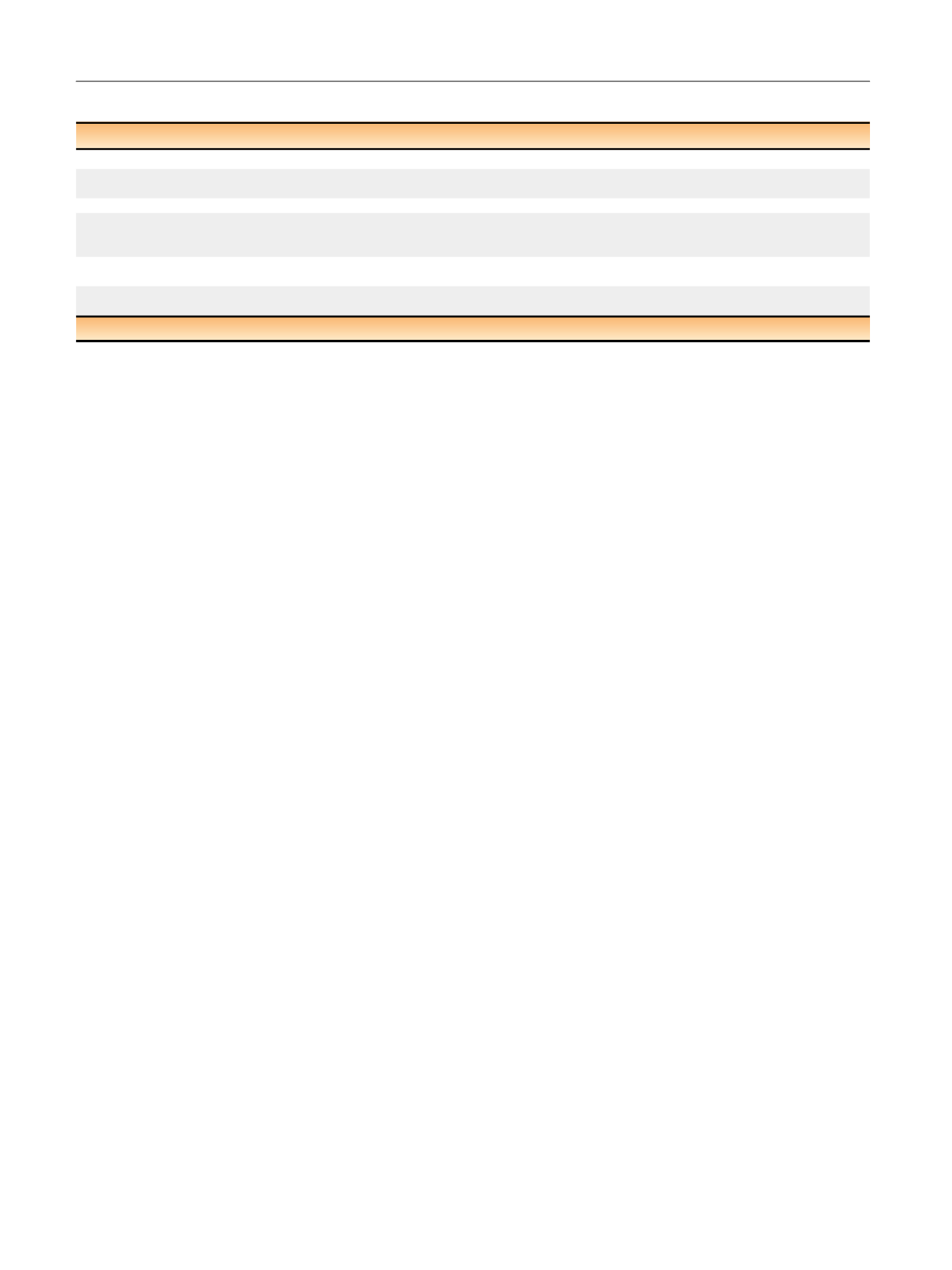
Table 1 – Definition of very-low and low-risk prostate cancer
Definition very low risk
Definition low risk
D’Amico et al 1998
[7]—
PSA
<
10 ng/ml, GS
<
7, & cT1–cT2a
European Association of Urology-ESTRO-SIOG
(Mottet et al 2016)
[8]—
PSA
<
10 ng/ml, GS
<
7, & cT1–cT2a
American Association of Urology
—
PSA
<
10 ng/ml, GS
<
7, & cT1–cT2a
National Comprehensive Cancer Network
(Carroll et al 2016)
[12]cT1c, GS
<
7, PSA
<
10 ng/ml, presence of disease in fewer than
3 biopsy cores,
50% PCa involvement in any core & PSA
density
<
0.15 ng/ml/g
cT1–cT2a, GS
<
7, PSA
<
10 ng/ml
Radiation Therapy Oncology Group
(Roach et al 2000)
[9]GS
<
6 & T1–2N0
GS
<
7 & T1–2Nx
Cancer of the Prostate Risk Assessment Score
(Cooperberg et al 2005)
[11]Age, PSA, clinical stage, biopsy GS, percentage of positive biopsy cores
GS = Gleason score; PCa = prostate cancer; PSA = prostate-specific antigen.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 2 3 8 – 2 4 9
240
















