
previous biopsy were not reported in the remaining eight
studies.
Characteristics of the studies are summarized in
Table 2 .MRI was performed using 3-T scanners in 16 studies
[16–18,20,24–33,35,36] ,1.5-T scanners in four studies
[19,21–23] ,and either 3 or 1.5 T in one study
[34] .Endor-
ectal coils were used in seven studies
[19,21–25,29] .In all
studies, the mpMRI protocol consisted of T2WI, DWI, and
DCE-MRI. The reference standard was radical prostatec-
tomy in five studies
[16,22,26,27,35] ,a combination of
systematic and targeted biopsies in seven studies
[17,20,23,25,29,34,36] ,and only targeted biopsy in seven
studies
[19,21,24,28,30,32,33]; the reference standard was
not consistent throughout the study population in two
studies
[18,31] .PI-RADSv2 scoring was performed by one to
five radiologists, either in consensus or independently. The
level of experience of the radiologists was heterogeneous,
ranging from 4 to 22 yr of experience in the prostate. In
most studies, the readers were blinded; however, in three
studies, the radiologists were aware that the patients had
biopsy-proven PCa
[22,26,35] ,and five studies were not
explicit regarding blinding
[18,19,30,32,36]. In the majority
of the studies, the interval between MRI and the reference
standard was less than 6 mo; however, the details were not
reported in 10 studies
[16–18,24,27–30,32,33]. PCa was
separately assessed according to zonal anatomy in seven
studies
[20,24,25,28,30,31,33] .However, in one study
[31],
only PCa in the PZ could be evaluated, as no detailed data
were provided in the article and the attempt to contact the
authors for provision of further information was unsuc-
cessful. Regarding the outcome assessed, seven studies
evaluated any cancer
[17,19,20,23,25,28,31,33], eight eval-
uated clinically significant cancer
[18,22,26,27,30,34–36],
and six evaluated both
[16,21,24,29,32] .With regard to
cutoff values, 13 studies used 4
[16,18–21,24– 28,30,31,35] ,four studies used 3
[32–34,36] ,and four
studies used both
[17,22,23,29] .The location of PCa was
separately reported by the PZ and TZ in six studies
[20,24,25,28,30,33].
3.3.
Quality assessment
Overall, the quality of the studies was not considered high,
mainly due to the patient selection domain
( Fig. 2).
Regarding the patient selection domain, there was generally
a high risk of bias as all but four of the studies were
retrospective in nature
[16–18,20–23,25–28,30,32– 36] .Seven studies were considered to have high concern
for applicability, as all or some of the patients had a
pathological
diagnosis of PCa prior to MRI
[16,17,22,26,27,32,35] .Regarding the index test domain,
there was a high risk of bias in nine studies. In three of nine
studies, reviewers were aware that patients had biopsy-
proven PCa
[22,26,35] .In the other six studies, the cutoff
value for determining PCa was not specified prior to
interpretation
[16,20,29,31,33,34] .Only one study had
concern for applicability, as PI-RADSv2 scores were
indirectly generated from existing clinical radiological
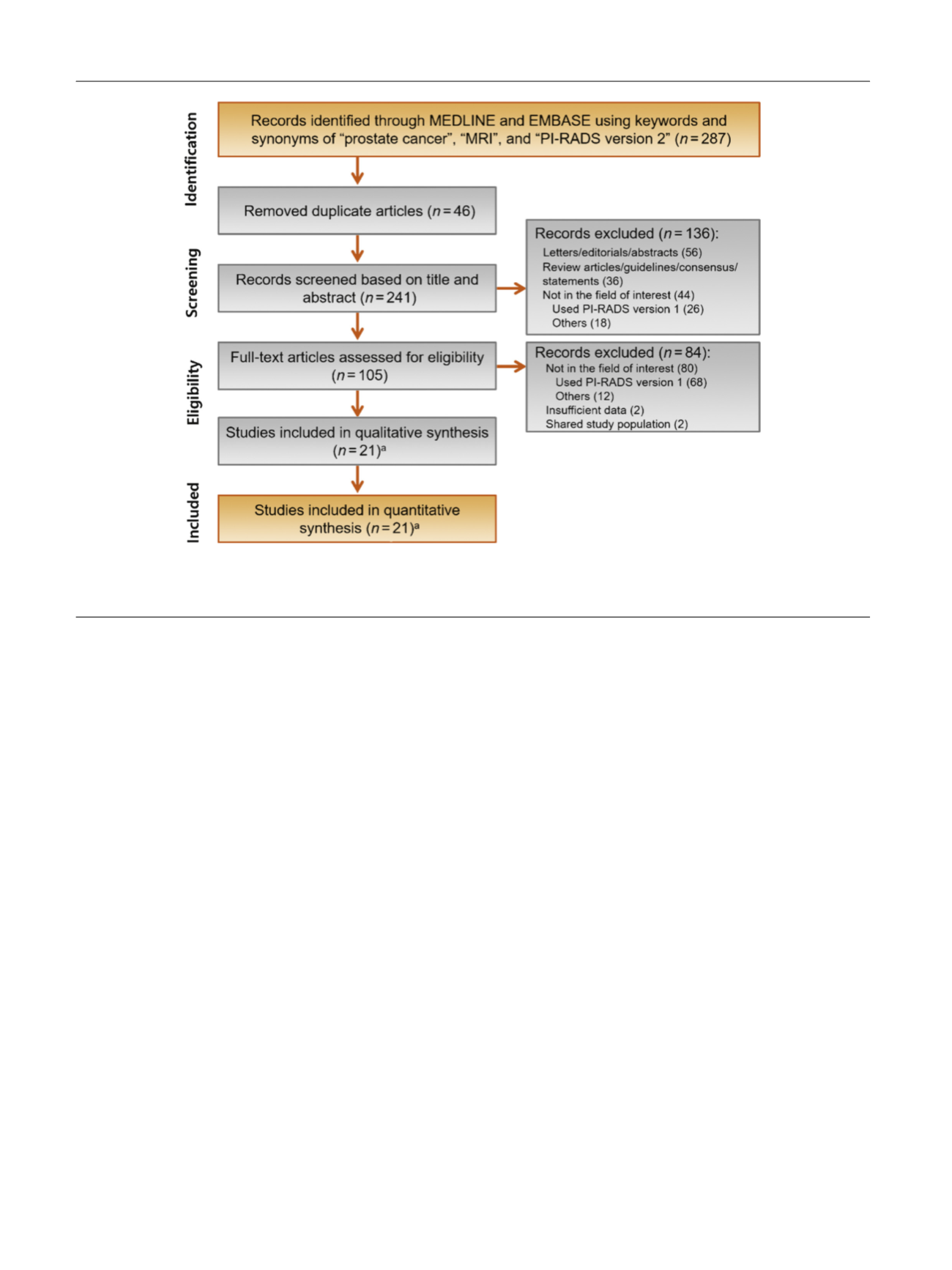
[(Fig._1)TD$FIG]
Fig. 1 – PRISMA flow diagram showing study selection process for meta-analysis.
a
Included original articles for qualitative and quantitative analyses
are references
[16–36] .MRI = magnetic resonance imaging; PI-RADS = Prostate Imaging Reporting and Data System; PRISMA = Preferred Reporting
Items for Systematic Reviews and Meta-analyses.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 1 7 7 – 1 8 8
180
















