
compared to AS within a particular race (eg, the difference
in mean EPIC scores between RP and AS among AA men).
Subsequently, we are able to formally test the interaction
between race and treatment by estimating how the effects
of treatment varied by race/ethnicity (eg, the difference in
mean EPIC scores between RP and AS among AA men
subtracted from the difference in mean EPIC scores between
RP and AS among white men, which is the DID). Using this
systematic approach, we were able to precisely test the
race-treatment interaction for all patient-reported func-
tional outcomes after prostate cancer treatment.
Other studies have examined the racial variation in
patient-reported quality-of-life outcomes after prostate
cancer treatment, but without testing the interaction
between race/ethnicity and treatment. Using the CaPSURE
data set, Lubeck et al
[17]demonstrated that significant
post-treatment differences in functional outcomes existed
between AA and white patients at 1 yr. Specifically, AA men
reported worse urinary and bowel function with corre-
spondingly worse bother scores at 1 yr after treatment.
However, unlike the current analysis, these models did not
adjust for baseline function or comorbidity. In a separate
prospective, longitudinal multicenter observational cohort,
the investigators found that AA men were more likely to
report better erectile function compared to white men at
2 yr after brachytherapy
[18]. However, this study and
many others in this space
[19,20]are limited by small
sample sizes of minority men, making their estimates less
reliable. Furthermore, these studies failed to test or even
allow for the interaction between race/ethnicity and
treatment; that is, these studies merely report what the
post-treatment differences are between races at a single
time point. In contradistinction, our study comprises a large
cohort of AA and Hispanic men. Furthermore, because our
study uses AS as a comparator, we were able to estimate
how the effect of treatment (as compared to AS) varies by
race/ethnicity. This approach allows more accurate estima-
tion of the patterns of risk for minority populations.
Despite these novel data, several limitations should be
acknowledged. First, clinically significant differences in
EPIC domain scores are not firmly established. We used
published thresholds when interpreting these data
[12] .Second, the racial classifications used in this study
are almost certainly inadequate for fully describing each
person’s true racial and ethnic identity, and may not fully
capture significant racial, social, and cultural distinctions.
Moreover, and more importantly, this racial/ethnic group-
ing is a fairly arbitrary construct. Our analysis does not
acknowledge the variability within each group; the
individuals’ characteristics may be much more important
than race/ethnicity. Third, this is an observational study,
and unmeasured confounding, such as differential clinician
experience, access to high-quality care, or use of pelvic floor
rehabilitation, may give rise to biased effect estimates. To
address these concerns, the CEASAR study contains a
comprehensive set of patient-level variables, which, in
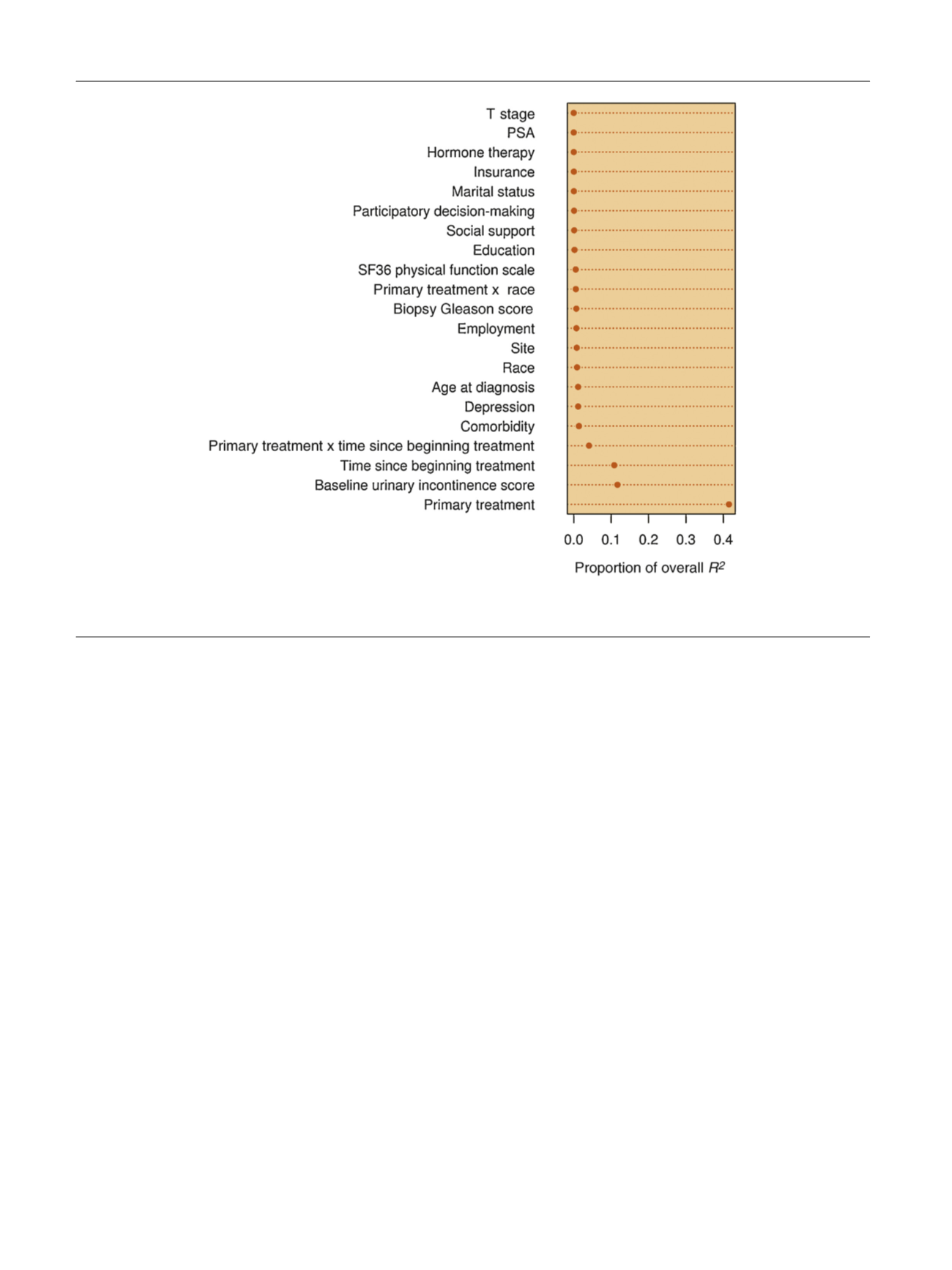
[(Fig._1)TD$FIG]
Fig. 1 – Proportion of overall
R
2
explained by different factors and interactions. PSA = prostate-specific antigen; SF36 = Short-Form 36-item
questionnaire.
E U R O P E A N U R O L O G Y 7 2 ( 2 0 1 7 ) 3 0 7 – 3 1 4
312
















